Heart disease kills women more than all forms of cancer combined. Yet, most women still don’t realize it’s their biggest health threat. In the U.S., about 1 in 5 female deaths is caused by heart disease - that’s roughly 307,000 women each year. And here’s the problem: many of these deaths could be prevented if symptoms were recognized earlier. But the symptoms women experience are often not what you see in movies or even what doctors are trained to look for.
It’s Not the Same as Men’s Heart Attack
When you think of a heart attack, you probably imagine someone clutching their chest, screaming in pain, collapsing. That’s the classic image - and it’s mostly based on how men experience heart attacks. But for women, it’s rarely that clear-cut. About 65% of women having a heart attack report chest pain. That means nearly 35% don’t feel chest pain at all. Instead, they get symptoms that feel more like the flu, stress, or just being worn out. Women are far more likely to have pain or pressure in their arms, jaw, neck, or back. One study found that 45% of women had arm or jaw pain during a heart attack, compared to just 28% of men. Shortness of breath is another big one - 42% of women report struggling to breathe, even when sitting still. Nausea, vomiting, and sudden dizziness are also common. Fatigue? That’s the silent warning sign. A study from Yale Medicine found that 71% of women who had heart attacks described extreme, unexplained fatigue - so bad they couldn’t make their bed or walk to the mailbox. Many dismissed it as just aging, stress, or lack of sleep. And it’s not just the symptoms that are different. The underlying heart problems are often different too. Men are more likely to have blocked major arteries. Women are more likely to have problems in the tiny arteries - called microvascular disease. These small vessels don’t show up on standard stress tests, so doctors often miss it. Women are also more prone to conditions like spontaneous coronary artery dissection (SCAD), where a tear forms in a heart artery without trauma or plaque buildup. And Takotsubo syndrome - sometimes called broken heart syndrome - happens far more often in women, especially after emotional stress.Why Diagnosis Gets Delayed - and Why It’s Deadly
When women walk into an emergency room with fatigue, nausea, and back pain, they’re often told they’re anxious, overworked, or have indigestion. A 2022 study in JAMA Internal Medicine found that 68% of women with cardiac symptoms were initially misdiagnosed as having psychological issues. This bias isn’t just outdated - it’s deadly. Women under 55 are seven times more likely than men to be sent home from the ER without proper testing. And within one year of being misdiagnosed, their chance of dying is 50% higher. Part of the problem is that women delay seeking help. The Family Heart Foundation found that women wait an average of 2.3 hours longer than men before calling 911. Why? Because they mistake their symptoms for something less serious. They think, “It’s just heartburn.” Or, “I’ve been stressed lately.” Or, “I’m just tired from caring for everyone else.” But when it comes to heart attacks, time is muscle. Every minute without blood flow damages the heart. That delay isn’t just inconvenient - it’s life-threatening. Even when women do get tested, the tools aren’t always right for them. Traditional stress tests and angiograms were designed using data from mostly male patients. A 2022 study showed that standard stress tests only catch coronary disease in 72% of women - but a newer test called Corus CAD, which looks at gene expression, catches it in 88% of women. That’s a huge difference. And yet, many hospitals still rely on outdated methods.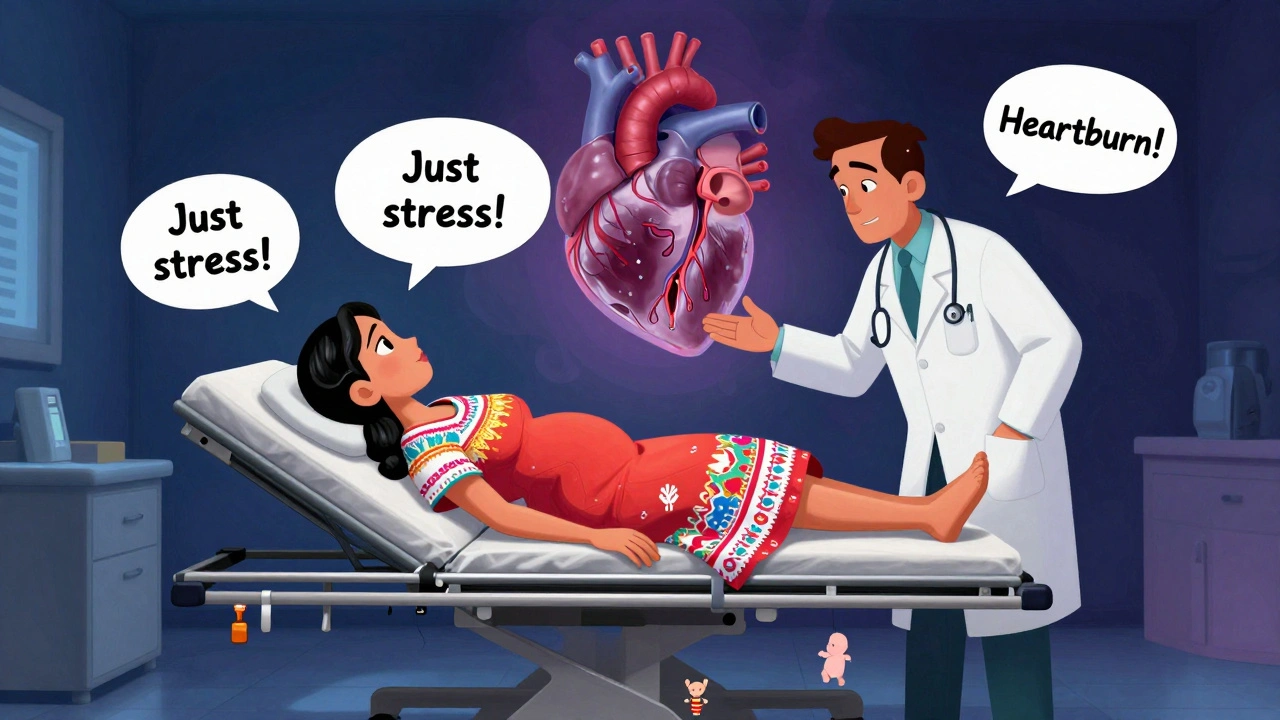
What Makes Women More at Risk
Some risk factors are the same for men and women - smoking, high blood pressure, high cholesterol, diabetes, obesity, and family history. But women have unique risk factors that men don’t. Pregnancy complications like preeclampsia, gestational diabetes, or delivering a baby prematurely can double or even triple a woman’s future risk of heart disease. Preeclampsia alone increases the risk by 80%, according to the National Heart, Lung, and Blood Institute. Menopause plays a big role too. Before menopause, estrogen helps protect the heart by keeping blood vessels flexible and lowering bad cholesterol. After menopause, that protection fades. Women over 65 are 34% more likely than men to have a “silent” heart attack - one with no obvious symptoms - because their body’s warning signals weaken. Mental stress is another major trigger. Women are 37% more likely than men to have chest pain triggered by emotional stress. Chronic stress, depression, and anxiety don’t just feel bad - they raise inflammation, increase blood pressure, and make arteries more prone to spasm. A 2023 study found that women who reported high levels of daily stress were twice as likely to develop heart disease within five years. And then there’s the research gap. For decades, heart studies focused on men. The original Framingham Heart Study, started in 1948, included only men. Even today, women make up just 38% of participants in major heart trials - despite being 51% of the population. That means a lot of what we know about heart disease is based on male biology. And that’s why women’s symptoms are still overlooked.How to Protect Yourself - Practical Steps
You can’t change your gender, your age, or your family history. But you can control many other factors. Here’s what actually works:- Know your numbers. Get your blood pressure, cholesterol, and blood sugar checked yearly - especially after 40. High blood pressure is the #1 silent killer in women.
- Track your pregnancy history. If you had preeclampsia, gestational diabetes, or delivered early, tell your doctor. These aren’t just pregnancy issues - they’re red flags for future heart disease.
- Pay attention to fatigue. If you’re exhausted for more than two weeks - and it’s not because you’re working late or caring for kids - get checked. Unexplained fatigue is the #1 warning sign in women.
- Don’t ignore jaw, arm, or back pain. If it comes on suddenly, doesn’t go away with rest, and feels different from muscle strain, don’t brush it off. Call 911.
- Manage stress. Daily meditation, walking, therapy, or even just saying no to extra obligations can lower your heart risk. Stress isn’t just mental - it’s physical.
- Ask for the right tests. If you have symptoms but a normal stress test, ask about the Corus CAD test or a coronary CT angiogram. These are better at catching microvascular disease.

When to See a Specialist
Not all cardiologists are trained in women’s heart health. Look for a provider who works at a Women’s Cardiovascular Center of Excellence. As of 2023, there are 147 certified centers across the U.S. These programs are required to reduce diagnostic delays for women by at least 25% compared to national averages. They use gender-specific protocols, understand SCAD and microvascular disease, and know how to interpret symptoms that don’t fit the male model. If you’ve had any of these: unexplained fatigue, chest tightness during stress, jaw pain with nausea, or shortness of breath with no clear cause - don’t wait. Go to a specialist. And if your doctor dismisses you, get a second opinion. Your life depends on it.The Bigger Picture
Heart disease costs the U.S. economy over $329 billion a year - and women account for 55% of those costs. Why? Because they tend to have longer hospital stays, more complications, and higher rates of heart failure after a heart attack. But this isn’t just a medical issue - it’s a systemic one. Research funding for women’s heart health is still only 34% of total cardiovascular spending. That’s not fair. And it’s not enough. Organizations like the American Heart Association’s Go Red for Women campaign have helped. Since 2004, awareness among women has risen from 44% to 70% - but we’re not there yet. The goal is 70% by 2030. That means more education, better training for doctors, and women speaking up about their symptoms. You don’t need to be a statistic. You don’t need to wait until it’s too late. If you’re a woman over 40 - or even younger with risk factors - know your body. Listen to it. Push for answers. Heart disease doesn’t care how strong you are. But you can care enough to fight for your health.What are the most common heart attack symptoms in women?
Women often experience symptoms that are different from the classic chest pain seen in men. Common signs include unusual fatigue, shortness of breath, nausea, vomiting, jaw or back pain, dizziness, and cold sweats. While chest discomfort can occur, it’s often described as pressure or tightness rather than sharp pain. About 35% of women have heart attacks without any chest pain at all.
Why are women’s heart attacks more deadly than men’s?
Women’s heart attacks tend to be deadlier because symptoms are often mistaken for less serious conditions like anxiety or indigestion. This leads to delays in treatment - on average, women wait 2.3 hours longer than men to seek help. Women are also more likely to have heart disease in small arteries (microvascular disease), which standard tests miss. Plus, women are more likely to be misdiagnosed in emergency rooms, and their hearts are more vulnerable to damage from delayed care.
Can pregnancy affect my future heart health?
Yes. Complications during pregnancy - like preeclampsia, gestational diabetes, or delivering a baby before 37 weeks - significantly increase your risk of heart disease later in life. Preeclampsia alone raises your risk by 80%. These conditions are signs that your blood vessels may not be functioning normally. Always tell your doctor about any pregnancy complications, even years later.
Is fatigue a real sign of heart disease in women?
Absolutely. Severe, unexplained fatigue - so intense it interferes with daily tasks like making your bed or walking to the mailbox - is one of the most common yet overlooked signs of heart disease in women. Studies show that 71% of women who had heart attacks reported this kind of fatigue weeks or months before the event. It’s not just being tired - it’s exhaustion that doesn’t go away with rest.
What tests should I ask for if I suspect heart problems?
If you have symptoms but a normal stress test, ask about the Corus CAD test, which analyzes gene expression and is 88% accurate in women. Also request a coronary CT angiogram to check for blockages in small arteries. Standard tests were designed for men and often miss microvascular disease, which is more common in women. Don’t accept a normal result if your symptoms persist.
Are there doctors who specialize in women’s heart health?
Yes. The American College of Cardiology certifies Women’s Cardiovascular Centers of Excellence. As of 2023, there are 147 such centers in the U.S. These programs are required to use gender-specific protocols and reduce diagnostic delays for women by at least 25%. If you have ongoing symptoms or risk factors, seek care at one of these centers.


Written by Guy Boertje
View all posts by: Guy Boertje