Most people with diabetes know their HbA1c number. It’s the lab test that tells you your average blood sugar over the past three months. But what if that number is hiding something dangerous? Two people can have the same HbA1c of 7.0%, yet one spends most of their day with blood sugar crashing below 70 mg/dL while the other rarely goes above 180 mg/dL. One is at high risk for fainting, seizures, or heart stress. The other is stable. HbA1c doesn’t tell you that. Time in Range does.
What Exactly Is Time in Range?
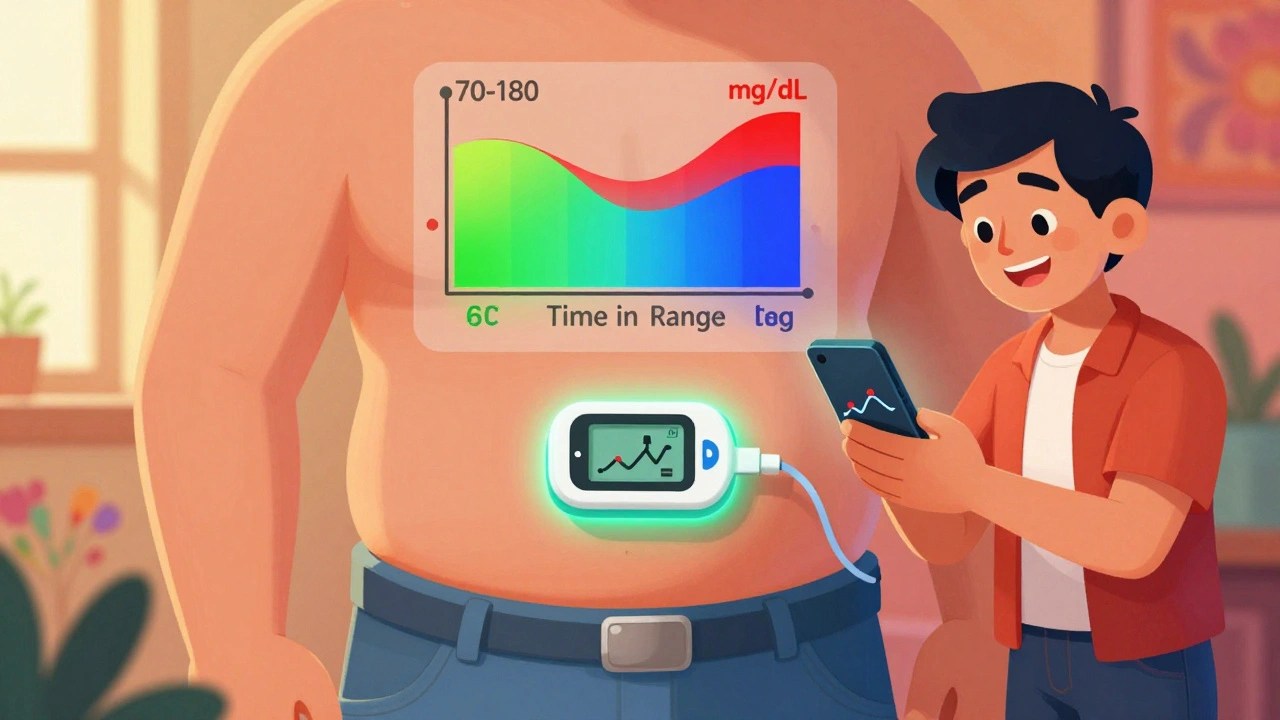
Time in Range (TIR) is the percentage of hours in a day your blood glucose stays between 70 and 180 mg/dL (3.9-10.0 mmol/L). It’s not a guess. It’s not a lab result from a finger prick. It’s calculated from data collected every 5 minutes by a continuous glucose monitor (CGM) worn on your arm or belly. Over 14 days, that’s up to 20,000 data points. When you wear your CGM properly, you get a clear picture: how much time you spend in range, too low, or too high.The goal? At least 70% of your day - that’s 17 out of 24 hours - in that sweet spot. That number lines up with an HbA1c of about 7%, but it’s far more useful. Why? Because it shows you when things go wrong. Did your sugar spike after lunch? Did it drop overnight after your evening walk? HbA1c can’t tell you that. TIR can.
Why TIR Beats HbA1c for Daily Control
Think of HbA1c like reading the summary of a book. You know the ending, but you miss all the drama in between. TIR is reading every chapter. It shows you the spikes, the crashes, the silent lows you didn’t feel.A 2023 Cleveland Clinic study found that two patients with identical HbA1c levels had wildly different TIR scores. One had 50% TIR - meaning they spent 12 hours a day with dangerous highs or lows. The other had 85% TIR. Same HbA1c. Totally different risks. The person with low TIR was far more likely to develop nerve damage, eye problems, or heart issues - even if their average looked fine.
That’s why the American Diabetes Association updated its 2025 Standards of Care to say CGM and TIR aren’t just for people on insulin anymore. If you’re taking metformin, GLP-1 agonists, or even just watching your carbs, you still need to know what your blood sugar is doing between visits. TIR helps you connect the dots between your food, your activity, your stress, and your meds - in real time.
How CGM Turns Data Into Action
Your CGM doesn’t just show numbers. It shows patterns. A bar graph on your phone tells you: 72% in range, 18% above, 10% below. But the real power comes from looking at the trend lines. Did your sugar climb after oatmeal? Did it dip after your 7 p.m. walk? Did your overnight low happen every Tuesday after wine?One patient in Cambridge noticed his glucose spiked every morning - even before breakfast. He blamed stress. But his CGM showed it only happened on days he skipped his evening protein snack. He started eating a small handful of almonds before bed. Within two weeks, his morning highs dropped by 40 points. His TIR jumped from 62% to 81%.
That’s the kind of insight HbA1c could never give you. It’s not about perfection. It’s about awareness. You don’t need to be in range 100% of the time. But knowing where you’re slipping lets you fix it - before it becomes a problem.

The Other Metrics That Matter
TIR isn’t the only number to watch. Your CGM also tracks:- Time Below Range (TBR): Time spent under 70 mg/dL. You want less than 4% - that’s less than an hour a day. Anything over 1% (15 minutes) increases hypoglycemia risk.
- Time Above Range (TAR): Time over 180 mg/dL. Aim for under 25%. More than 40% means you’re spending too much time in danger zone.
- Glucose Variability: How much your numbers swing. High swings mean your body is struggling to stabilize. A coefficient of variation over 36% is a red flag.
- Time in Tight Range (70-140 mg/dL): Some people, especially those in research or with prediabetes, aim for this tighter zone. It’s harder, but it may reduce long-term damage.
These numbers together paint the full picture. If your TIR is 75% but your TBR is 8%, you’re having dangerous lows you might not feel. If your TAR is 30%, you’re damaging your blood vessels even if your HbA1c is “good.”
Who Should Be Using CGM and TIR?
For years, CGM was only for people on insulin. That changed in 2025. The ADA now says any adult with type 2 diabetes on glucose-lowering meds - even metformin or sulfonylureas - should consider CGM. Why? Because high blood sugar, even without insulin, still causes damage. And many people don’t know they’re spiking after meals.Here’s who benefits most:
- People with frequent lows (even if they don’t feel them)
- Those with HbA1c that doesn’t match how they feel
- Anyone struggling with post-meal spikes
- People on GLP-1 drugs like semaglutide - these can cause lows if diet isn’t adjusted
- Those with prediabetes trying to reverse it
Even if you’re not on meds, knowing your TIR can help you understand how your body responds to food, sleep, and stress. It’s not just for treatment - it’s for prevention.

Getting Started: What You Need to Know
You don’t need to be a tech expert. But you do need to know how to use the data.First, get a CGM. Dexcom, Abbott, and Medtronic are the main brands. Most work for 10-14 days. Wear it continuously. Don’t peel it off early. You need at least 70% of the time active - so if you’re wearing it for 14 days, that’s 10 full days of data.
Then, review your report. Most apps show a daily graph. Look for:
- Consistent spikes after certain meals
- Low periods after exercise
- Highs in the morning (dawn phenomenon)
- Weekend patterns vs. weekdays
Bring this to your doctor. Don’t just say, “My sugar’s high.” Say, “I’m at 68% TIR. I spike after pasta every night. My TBR is 5% - I had three lows last week, and I didn’t feel any.” That’s actionable.
Most people need one or two visits to learn how to interpret the graphs. After that, it becomes second nature. Many users say the biggest win isn’t better numbers - it’s peace of mind.
Barriers and Real-World Challenges
It’s not perfect. CGMs cost money. Insurance coverage is improving, especially since the 2025 ADA guidelines, but it’s still a hurdle in many places. In the UK, NHS access varies by region. In the US, Medicare now covers CGM for type 2 patients on insulin or those with frequent lows - but not always for others.Sensors can itch. They can fall off. The app can be overwhelming. Some people feel paralyzed by too much data. That’s normal. Start small. Look at your TIR for one week. Don’t try to fix everything at once.
One woman in Cambridge told me she deleted her app for three weeks because it stressed her out. When she came back, she only looked at her weekly TIR summary - not the hourly graphs. Her number went from 58% to 74% in two months. Sometimes, less is more.
The Future Is Here
CGM use among Medicare beneficiaries with type 2 diabetes jumped from 15% in 2019 to 42% in 2023. The global market is expected to hit $18.6 billion by 2030. Why? Because it works.Research is now linking TIR directly to complication risk. A 2025 study in the Journal of Clinical Endocrinology & Metabolism found that every 10% increase in TIR reduced the risk of retinopathy by 40%. That’s huge.
Future tools will use AI to suggest changes: “Your sugar spikes after rice. Try swapping half for lentils.” Or, “You’re low after yoga. Have a 10g carb snack before class.”
Time in Range isn’t a fad. It’s the next step in diabetes care. It turns abstract numbers into real, daily control. It gives you power over your body - not just reports from a lab.
If you have diabetes, and you’re not using CGM, you’re flying blind. HbA1c is a snapshot. TIR is the full movie. And you deserve to see it all.

Written by Connor Back
View all posts by: Connor Back