Comprehensive Understanding: Asthma and Obstructive Pulmonary Disease
As a health-conscious guy named Caspian, who double as a researcher and a father, I find respiratory diseases increasingly intriguing. Just as how our pet beagle, Finn, is highly susceptible to specific health issues like ear infections, humans have their vulnerabilities too. Asthma and obstructive pulmonary diseases frequently fall into these categories, imposing a significant burden on many lives across the globe. Do not confuse these two conditions as one because they are as different as night and day in several aspects, yet ironically, they share a cryptic bond. Intriguing, isn't it? Let's dive into this health puzzle and unravel the mystery linking obstructive pulmonary disease and asthma.
Details on Asthma: Not Just an Ordinary Cough
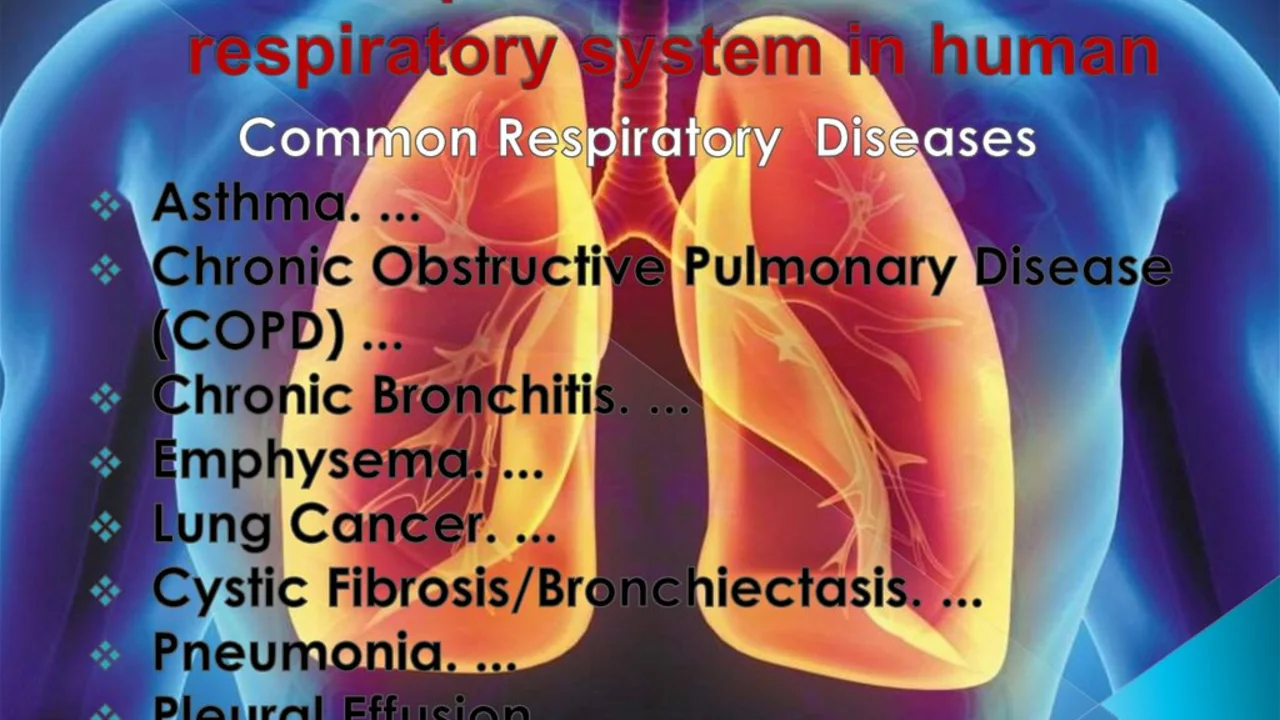
So what is asthma? It's not that grumbling made by your stomach when it shouts for food or the howl of Finn when he sees a squirrel. It's a more persistent and nagging issue. Asthma is a chronic inflammatory condition affecting your airways. Imagine having inflamed breathing tubes, creating a perfect party ground for mucus to pile up and then having your airways contract in reaction. Yes, it's as bad as it sounds. This results in symptoms like wheezing, shortness of breath, and coughing, rather similar to the noises my daughter Layla tries to replicate with her kids' instrument set but much more distressing. The greater mystery here lies in its link with another infamous respiratory disease - obstructive pulmonary disease.
The Explanation: Obstructive Pulmonary Disease
Now, picturing how obstructive pulmonary disease works isn’t too far off from how Finn acts when he spots a squirrel from afar. Your airways and air sacs lose their elastic quality, kind of like an older rubber band that’s stretched out one too many times. The walls in between the air sacs are destroyed, walls thicken with inflammation, or your airways make more mucus than the time Layla tried to make slime at home. This hinders air flow, induces shortness of breath and breeds many other symptoms reminiscent of an aged Finn struggling to catch his foe.
Discovering the Intricate Link: Asthma and Obstructive Pulmonary Disease
Perhaps we can think about it like this: Asthma is like Layla on her sugar highs, impulsive and all over the place with a sudden onset, and obstructive pulmonary disease more like Finn in his later years, a progressive condition that slowly limits his activities. But they have a surprising link. Known as 'Asthma-Obstructive Pulmonary Disease Overlap,' this condition presents characteristics of both these diseases in one person. It's like the typical superhero-villain crossover episode we secretly all love. Detecting ACO can be as complex as understanding Layla's teenage lingo, but it plays a crucial role in managing respiratory health effectively since it's more severe and incurs higher medical costs.
Keeping Your Airways Clear: Fighting Against Respiratory Diseases
Having an obstructive lung condition isn’t like winning the lottery. It's more similar to Finn's potty training days, frustrating and may seem never-ending at first. However, just as Finn eventually mastered the art of not making a mess, there's hope for those with these respiratory conditions. They can be managed with a combination of lifestyle changes, proper medication, and regular medical check-ups. It may be a bit more challenging than teaching my daughter Layla algebra, but it's possible and necessary. Breathing is one of the fundamental aspects of life, so remember to care for your lungs as much as you would for your pet or child.
Now that we've embarked on this knowledge-filled adventure, we have a responsibility not just to ourselves, but also to those around us, to spread the word and increase awareness about these interlinked respiratory conditions. So next time when you explain asthma to someone, make sure not to leave out its sibling – obstructive pulmonary disease.

Written by Guy Boertje
View all posts by: Guy Boertje