Time in Range: What It Means for Diabetes Management and How to Improve It
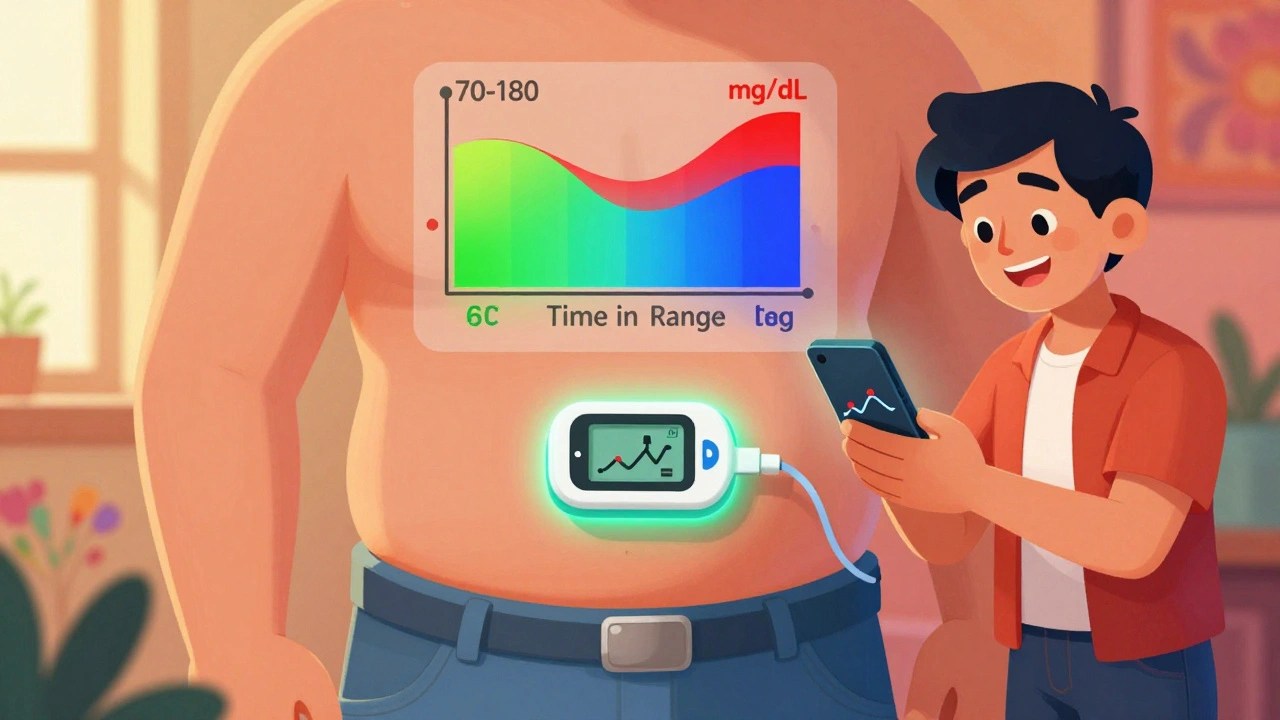
When you hear time in range, the percentage of hours your blood glucose stays between 70 and 180 mg/dL. Also known as glucose time in range, it’s becoming the new standard for tracking how well diabetes is controlled—not just on paper, but in real life. Unlike A1C, which gives you an average over months, time in range shows you exactly how often your numbers stay safe. That means fewer lows, fewer highs, and less guesswork. If you’re using a CGM, a continuous glucose monitor that tracks your sugar levels every few minutes. Also known as continuous glucose monitoring, it’s the tool that makes this metric possible. You don’t need to be a tech expert to use it. Most devices sync with your phone and give you daily reports—no lab visits required.
Why does this matter? Because staying in range isn’t just about avoiding complications. It’s about energy, focus, sleep, and mood. When your blood sugar swings wildly, you feel it: brain fog, crashes, irritability. But when you spend more time between 70 and 180, you start noticing small wins—like not needing a nap after lunch, or sleeping through the night without waking up shaky. People who track this closely often cut their insulin doses, reduce hypoglycemia episodes, and feel more in control. It’s not magic. It’s data. And it’s personal. Your target range might be slightly different based on age, activity level, or other health conditions. But the goal stays the same: more hours in the zone, fewer spikes and drops.
Time in range connects directly to the tools and choices you make every day. It’s affected by what you eat, when you move, how you take your meds, and even how you sleep. That’s why posts here cover things like generic maintenance medications, cost-effective drugs that help keep glucose stable long-term. Also known as generic diabetes drugs, they’re often the backbone of daily treatment. You’ll find advice on avoiding dangerous interactions, like how azoles and tacrolimus, a combination that can spike blood sugar in transplant patients. Also known as azole-tacrolimus interaction, it’s a reminder that some meds don’t play nice with glucose control. You’ll see how therapeutic drug monitoring, tracking blood levels of meds like tricyclics or insulin. Also known as TDM, it helps fine-tune doses so you stay in range safely. And you’ll learn how apps and comparison tools help you find affordable generics without sacrificing quality.
There’s no one-size-fits-all path to better time in range. But the data doesn’t lie. If you’re checking your numbers regularly, you’re already ahead. The posts below give you real strategies—what works, what doesn’t, and what to watch out for. Whether you’re just starting with CGM or have been managing diabetes for years, you’ll find something that helps you live better, not just survive.
Time in Range: How CGM Metrics Help You Manage Diabetes Daily
Time in Range (TIR) uses continuous glucose monitoring to show how often your blood sugar stays in a healthy zone - giving you real-time control over diabetes, beyond what HbA1c can tell you.
- Dec 4, 2025
- Connor Back
- 8