Generic Substitution: What It Is, Why It Matters, and How It Saves You Money
When you pick up a prescription, you might see a different name on the bottle than what your doctor wrote. That’s generic substitution, the practice of replacing a brand-name drug with a chemically identical version approved by health regulators. Also known as generic switching, it’s one of the most common ways to cut drug costs without losing effectiveness. It’s not a trick or a shortcut—it’s science. The FDA and Health Canada require generic drugs to have the same active ingredient, strength, dosage form, and route of administration as the brand version. They must also prove they work the same way in your body. That’s why millions of people use generics every day—and why pharmacies are encouraged to swap them in unless your doctor says no.
But not all substitutions are the same. Some drugs, like antiretroviral HIV medications, complex treatments where tiny differences in absorption can affect resistance, need extra care. Others, like corticosteroids, used for inflammation and immune conditions, can be risky if switched without proper tapering. Then there are drugs where the difference is negligible—like atenolol, a common blood pressure pill, or progesterone, used in fertility and menopause care. These are the ones where generic substitution shines: safe, predictable, and hundreds of dollars cheaper.
Behind every generic drug is a story about how production works. Brand-name companies spend millions on marketing and patents. Generic makers don’t. They focus on efficient manufacturing—often overseas, at scale, with smarter labor use. That’s why a 30-day supply of brand-name Lipitor might cost $300, while its generic version, atorvastatin, runs under $10. The pill looks different? So what. The active ingredient is identical. What changes is your wallet.
Still, people worry. What if the filler ingredients cause a reaction? What if the absorption is off? That’s where therapeutic equivalence comes in. Health agencies rate generics with codes like AB1, AB2—meaning they’re interchangeable. Your pharmacist checks these ratings before swapping. And if you’ve had bad reactions before? Tell them. Not all generics are made equal in formulation, even if the active drug is the same.
Some drugs, like liquid antibiotics or injectables, need special attention. A dosing error with an oral syringe can be dangerous—especially when switching brands. That’s why pharmacies now train staff on accurate milliliter measurements. It’s not just about the drug. It’s about how you take it.
And here’s the thing: generic substitution isn’t just a cost-saver. It’s a system that keeps healthcare running. When hospitals face shortages of injectable drugs like epinephrine or cisplatin, generics often fill the gap. When cancer patients need oral chemo like capecitabine, generics make long-term treatment possible. When someone with Bell’s palsy needs prednisone, or someone with acne needs clindamycin gel, generics mean they don’t have to choose between medicine and rent.
What you’ll find below are real, practical guides on how generic substitution affects everyday treatments—from antidepressants to antifungals, from blood pressure pills to skin creams. Some posts show you how to compare alternatives. Others warn you about interactions with supplements or foods. A few dive into the hidden costs of drug production. Together, they give you the full picture: not just what generic substitution is, but how it touches your life, your health, and your budget—every single day.
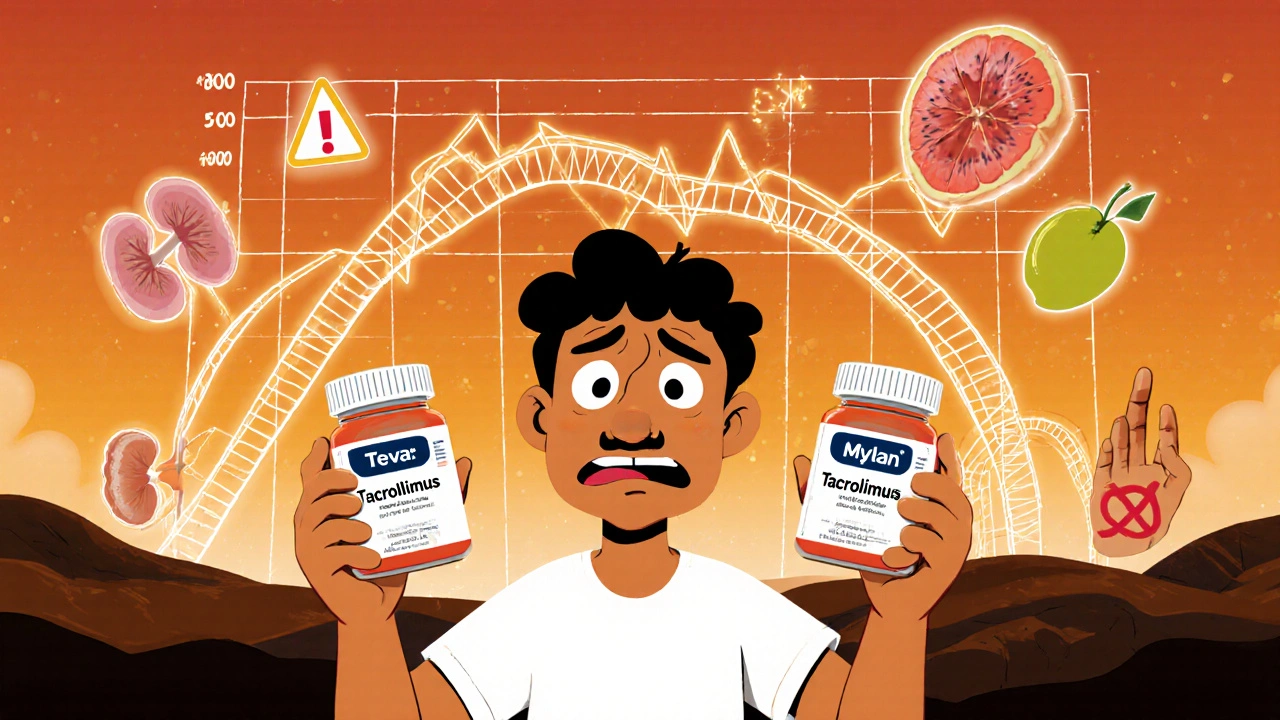
Immunosuppressants: Cyclosporine and Tacrolimus Generic Issues
Generic versions of cyclosporine and tacrolimus save money but carry risks for transplant patients due to narrow therapeutic windows. Learn why switching between generics can cause rejection or toxicity-and how to protect your transplant.
- Nov 24, 2025
- Connor Back
- 13