Generic Medication Errors: What Goes Wrong and How to Stay Safe
When you pick up a generic medication, a lower-cost version of a brand-name drug that contains the same active ingredient. Also known as generic drugs, it works the same way as the brand version—but not always in the same way for your body. That’s the problem. Generic medications save money, but they’re not always interchangeable without risk. For some drugs, even tiny differences in how they’re made can lead to serious side effects, treatment failure, or worse. These are called generic medication errors, mistakes that happen when generic drugs are switched, misdosed, or misunderstood by patients or providers. They’re not rare. They’re quietly happening in homes, clinics, and hospitals every day.
One big reason? Narrow therapeutic index, when the difference between a helpful dose and a harmful one is very small. Also known as NTI drugs, these include medications like cyclosporine, tacrolimus, and warfarin. For transplant patients, switching from one generic version of cyclosporine to another—even if both are FDA-approved—can trigger organ rejection. Why? Because the body absorbs each version slightly differently. It’s not about quality. It’s about bioequivalence. And not all generics are created equal when your life depends on precise blood levels. Then there’s dosing accuracy, how correctly a medication is measured and taken. For liquid medicines, using a kitchen spoon instead of an oral syringe can mean giving 20% too much—or too little. That’s not a typo. That’s a real risk, especially for kids, seniors, and people on multiple drugs. Even simple things like confusing milligrams with micrograms, or missing a dose because the pill looks different this month, add up. And when you’re on antidepressants, ACE inhibitors, or antiretrovirals, those small errors can spiral into hospital visits.
Therapeutic drug monitoring helps, but it’s not automatic. You have to ask for it. If you’re on tricyclic antidepressants or immunosuppressants, your doctor should be checking your blood levels—not just prescribing and hoping. But most people don’t know this is an option. And pharmacies? They’re under pressure to swap generics quickly and cheaply. That’s not always bad—but it’s not always safe either. The system isn’t broken. It’s just missing guardrails. You need to be your own advocate: know your meds, ask if your generic is the same as last time, use the right dosing tools, and speak up if something feels off.
Below, you’ll find real stories and clear guides on how these errors happen—and how to stop them. From why your blood pressure med stopped working after a refill, to how a simple syrup bottle nearly caused a child’s overdose, to what to do when your HIV meds change shape. These aren’t hypotheticals. They’re happening. And you can protect yourself.
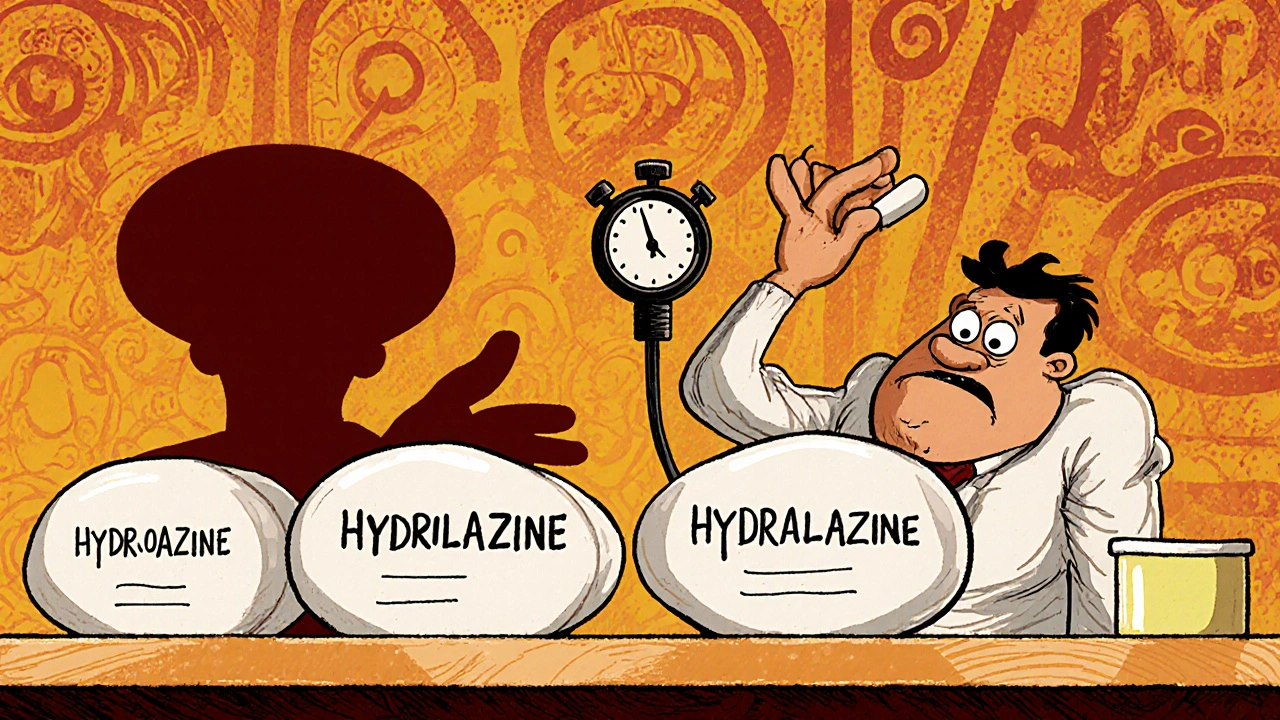
Medication Errors with Generics: Look-Alike, Sound-Alike Risks and How to Stop Them
Look-alike, sound-alike generic drugs cause thousands of preventable medication errors each year. Learn how similar names and packaging lead to dangerous mix-ups-and what patients and providers can do to stop them.
- Nov 27, 2025
- Guy Boertje
- 8