Every year, thousands of people in the U.S. are harmed-not by the medicine they need, but by the one they get by mistake. And it’s not because someone made a careless mistake. It’s because two drugs look too much alike, or sound too much alike. This is especially true with generic medications, where dozens of manufacturers produce pills that can be nearly identical in color, shape, and name. The result? Confusion that leads to dangerous errors.
What Are Look-Alike, Sound-Alike (LASA) Drugs?
Look-alike, sound-alike (LASA) drugs are medications whose names or packaging are so similar that they can be easily mixed up. This isn’t just about spelling. It’s about how they look on a shelf, how they sound when a nurse reads them aloud, or how they appear on a computer screen during prescribing.
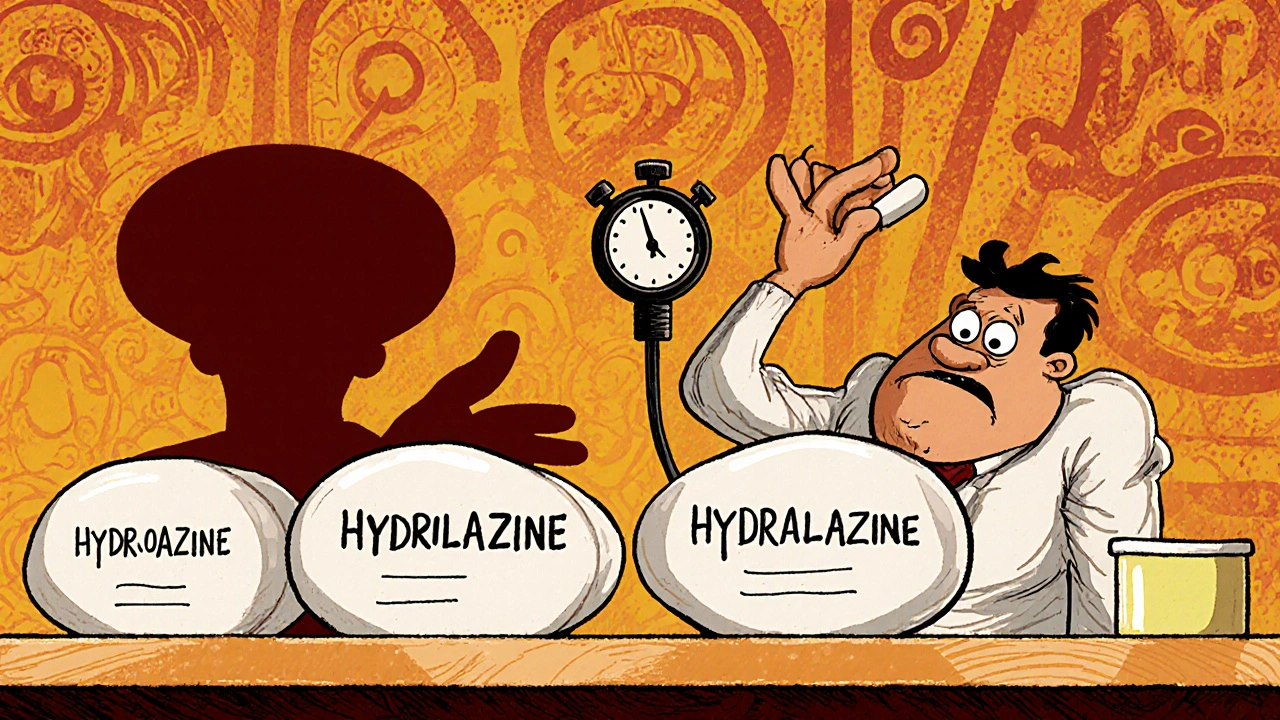
Take hydroxyzine and hydralazine. One treats anxiety and itching. The other lowers blood pressure. But if a pharmacist grabs the wrong bottle-or a nurse hears “hydra” instead of “hydro”-the consequences can be deadly. A patient expecting a sedative gets a powerful vasodilator instead. Blood pressure crashes. Organs fail.
Another common pair: albuterol (for asthma) and atenolol (for heart rhythm). Say them out loud. They’re almost the same. In a noisy ER, that mix-up happens more often than you think.
And it’s not just names. Packaging matters too. Two generics for different conditions might both come in white, oval, 10 mg capsules. Same size. Same imprint. Same bottle. The only difference? A tiny font on the label. That’s not enough.
Why Generics Are the Biggest Problem
Brand-name drugs usually have unique packaging. The company spends millions to make their product stand out. But generics? They’re made by dozens of companies, all trying to cut costs. The result? Similar shapes. Similar colors. Similar labels.
There are nearly 1,000 known LASA pairs in the U.S. alone, according to the Institute for Safe Medication Practices (ISMP). And about 25% of all medication errors are linked to these confusing names or appearances. That’s one in four.
Generic drugs make up over 90% of prescriptions filled in the U.S. That means the chance of a LASA error isn’t rare-it’s routine. And it’s getting worse. New generic versions hit the market every month. Many are approved without enough scrutiny of how their name might clash with existing drugs.
The FDA rejected 34 drug names in 2021 alone because they were too similar to existing ones. But that’s just the tip of the iceberg. Most generic names slip through. And once they’re on the shelf, it’s too late.
Where Do These Errors Happen?
LASA errors don’t happen in one place. They creep in at every step:
- Prescribing: A doctor types “Valtrex” but means “Valcyte.” Both are antivirals for transplant patients. One treats herpes; the other prevents a deadly CMV infection. Mix them up, and the patient gets the wrong treatment.
- Dispensing: A pharmacist pulls a bottle off the shelf. The label looks right. The name looks right. But it’s the wrong drug. This happens more than you’d think-especially during busy shifts.
- Administration: A nurse hears “dopamine” and gives “dobutamine.” Both are IV drugs used in ICUs. One boosts heart output. The other raises blood pressure. Give the wrong one, and a patient can go into cardiac arrest.
Studies show 68% of medication errors happen during administration. That’s when the drug is actually given to the patient. By then, it’s too late to catch the mistake.

Real Cases, Real Harm
In 2018, a 72-year-old woman in Florida was given hydralazine instead of hydroxyzine. She had a history of low blood pressure. Within minutes, her BP dropped to 60/30. She was rushed to the ICU. She survived-but barely.
Another case: a child was given quinine (for malaria) instead of quinidine (for irregular heartbeat). Quinine is toxic at low doses in children. The child suffered hearing loss and kidney damage.
These aren’t outliers. They’re predictable. The UK’s National Reporting and Learning System recorded over 200,000 medication incidents in one year. Of those, 66 were fatal. Many involved LASA drugs.
What’s Being Done-And What’s Not Working
There are solutions. But most hospitals don’t use them fully-or at all.
Tall man lettering is one of the most effective tools. Instead of writing “prednisone” and “prednisolone,” you write “predniSONE” and “predniSOLONE.” The capital letters highlight the difference. A 2020 study found this reduced errors by 67% across 12 hospitals.
Another fix? Physical separation. Keep LASA drugs on different shelves. Don’t put them side by side. Simple. Cheap. Effective.
But here’s the problem: most pharmacies still store generics in alphabetical order. That means “hydroxyzine” and “hydralazine” are right next to each other. No wonder mistakes happen.
Barcode scanning helps-but only if the system is smart enough to flag LASA pairs. Many hospital systems still don’t have that capability. And even when they do, alerts can be ignored. Too many false alarms. Nurses get “alert fatigue.”
Electronic health records (EHRs) are supposed to help. But most still let you scroll through long lists of drug names. If “albuterol” and “atenolol” appear next to each other, the prescriber might click the wrong one without even noticing.

The Best Fixes Are Already Here
Some hospitals are getting it right.
A system in Ohio started using AI-powered alerts in their EHRs. When a doctor typed a drug name, the system scanned for LASA matches. If there was a risk, it blocked the order and forced a double-check. In six months, LASA errors dropped by 82%. False alerts? Only 1.3%.
Another hospital in Minnesota added color-coded labels for high-risk drugs. Hydroxyzine got a blue label. Hydralazine got a red one. Pharmacists reported a 45% drop in errors within three months.
And it’s not just hospitals. Some pharmacies now use “do not confuse” lists. They print them out. Put them on the counter. Train staff to check them before filling any prescription.
The key? It’s not about blaming the person. It’s about fixing the system.
What Patients Can Do
You’re not powerless. Here’s what you can do:
- Know your drugs. Don’t just take what’s handed to you. Ask: “What is this for?” and “Why this one?”
- Check the label. Does the name match what your doctor told you? Does the pill look the same as last time? If not, ask.
- Use one pharmacy. If you fill all your prescriptions at one place, they’ll spot a problem before it happens.
- Ask for brand names if you’re unsure. If you’ve had a bad reaction to a generic before, say so. You have the right to ask for the brand.
And if you’re on multiple medications? Bring a list to every appointment. Don’t rely on memory. Write it down. Include the dose and why you take it.
The Bigger Picture
Medication errors cost the U.S. healthcare system over $42 billion a year. LASA errors are a huge part of that. And they’re preventable.
The FDA, WHO, and ISMP all agree: this isn’t about human error. It’s about poor design. Bad labeling. Lack of standards. We accept it because it’s always been this way. But it doesn’t have to be.
Regulators need to enforce stricter naming rules. Pharmacies need to separate high-risk drugs. Hospitals need AI alerts that actually work. And patients need to speak up.
By 2025, the FDA aims to cut LASA errors in half. That’s possible-if we stop treating this as a mystery and start treating it like the solvable problem it is.
It’s not about being perfect. It’s about being smarter. One label change. One shelf reorganization. One alert system. One patient asking a question. Those small things add up.
Next time you pick up a prescription, take a second look. The right medicine could be one detail away.

Written by Guy Boertje
View all posts by: Guy Boertje