Generic Drug Confusion: Why Switching Brands Can Go Wrong
When you hear generic drug confusion, the uncertainty and risks that arise when patients switch between different versions of the same medication. Also known as generic substitution, it's a common practice meant to cut costs—but not all generics are created equal. For most drugs, it works fine. But for others, even tiny differences in how the body absorbs the medicine can mean the difference between healing and harm.
Take cyclosporine, an immunosuppressant used after organ transplants. A small change in blood levels—just 10%—can trigger organ rejection. The same goes for tacrolimus, another critical transplant drug with a narrow therapeutic window. These aren’t like painkillers or antibiotics. They demand precision. And when pharmacies swap one generic for another without telling you, your body might not know the difference—but your health will.
Then there’s therapeutic drug monitoring, the process of measuring drug levels in your blood to ensure they’re in the safe, effective range. It’s not routine for most prescriptions, but for people on drugs like tricyclic antidepressants or antiretrovirals, skipping it can be risky. Even if your doctor says the generic is "the same," your body might react differently. That’s why tracking symptoms, side effects, and lab results matters more than ever.
And it’s not just about the drug itself. drug interactions, when one medication changes how another works in your body can turn a safe generic into a problem. A common blood pressure pill like lisinopril might seem harmless, but if you’re eating more bananas or spinach because you’re trying to be healthy, your potassium levels could spike. Same with herbal supplements like St. John’s Wort messing with antidepressants. Generics don’t change the chemistry—but they do change the context.
Many people assume all generics are identical because they have the same active ingredient. But fillers, coatings, and manufacturing processes vary. That’s why some patients feel worse after switching—even if their pharmacy says it’s "equivalent." The FDA allows a 20% variation in absorption, and for some drugs, that’s too wide a margin. You’re not imagining it. You’re not being dramatic. You’re just paying attention.
So what can you do? Ask your pharmacist if the generic you’re getting is the same brand as last time. Check your prescription label for the manufacturer name. If you’re on a critical medication, ask your doctor about therapeutic drug monitoring. Don’t let cost savings override safety. And if you notice new side effects after a switch—fatigue, dizziness, mood changes, or worse—don’t wait. Talk to your provider. Your body is telling you something.
The posts below dive into real cases where generic drug confusion led to serious consequences—and how people found safer, smarter ways to manage their meds. From HIV treatments to transplant drugs, from liquid dosing errors to apps that track your prescriptions, you’ll find clear, practical advice that actually helps. No fluff. Just what you need to stay safe while saving money.
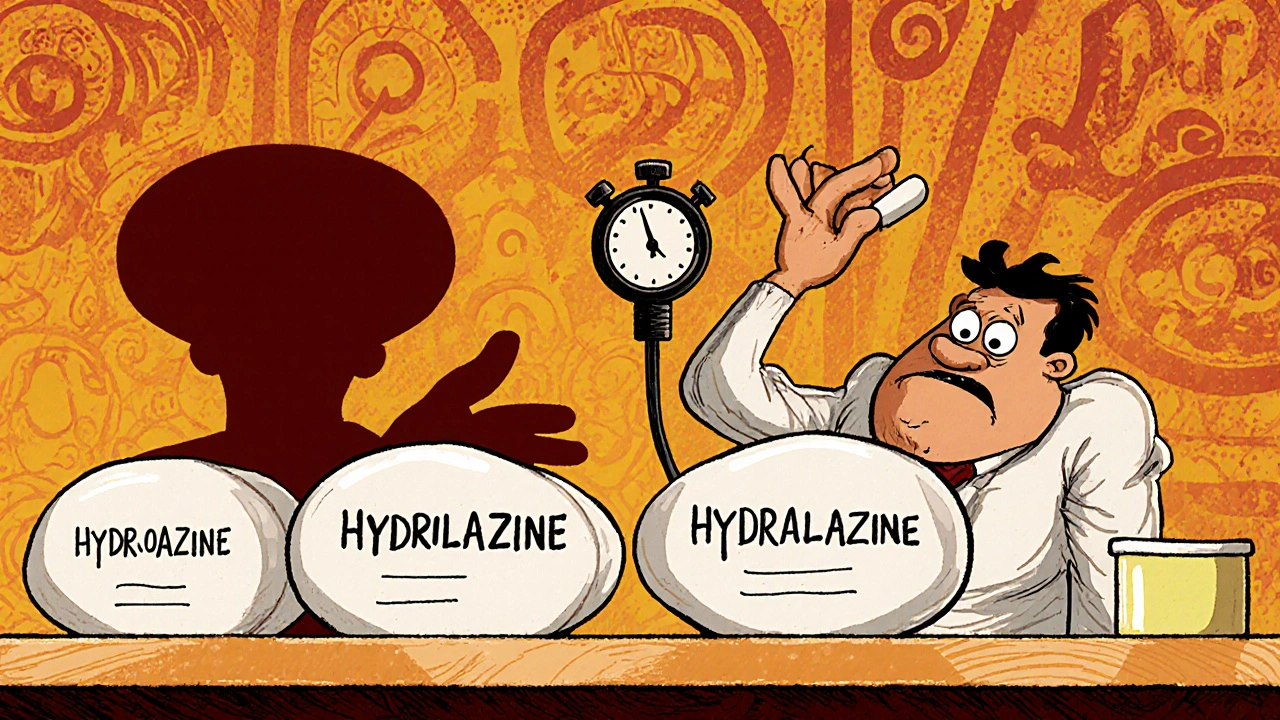
Medication Errors with Generics: Look-Alike, Sound-Alike Risks and How to Stop Them
Look-alike, sound-alike generic drugs cause thousands of preventable medication errors each year. Learn how similar names and packaging lead to dangerous mix-ups-and what patients and providers can do to stop them.
- Nov 27, 2025
- Guy Boertje
- 8