Diabetes Management: Practical Tips for Controlling Blood Sugar and Avoiding Complications
When you’re living with diabetes management, the daily process of keeping blood sugar levels stable to prevent long-term damage to organs and nerves. Also known as blood sugar control, it’s not just about taking pills or shots—it’s about making choices that add up over time. Many people think diabetes is only about sugar intake, but it’s really about how your body handles insulin, what medications you take, and how stress, sleep, and even weather affect your numbers.
Insulin therapy, the use of injected or inhaled insulin to replace or supplement the body’s natural insulin production is a key part of diabetes management for many, especially those with type 1. But even for type 2, where insulin isn’t always needed right away, the right medication—whether brand or generic—can make a huge difference. Generic versions of metformin, glimepiride, and insulin analogs save money without cutting corners on safety, as long as you stick to one brand and avoid switching unless your doctor says it’s safe. Some people feel worse after switching generics, not because the drug is weaker, but because small changes in absorption can throw off their balance. That’s why tracking your numbers daily matters more than ever.
Type 2 diabetes, a chronic condition where the body becomes resistant to insulin or doesn’t make enough doesn’t have to mean giving up everything you love. It means learning what foods spike your sugar, how exercise lowers it naturally, and when to check your levels before, during, or after activity. A 20-minute walk after dinner can drop your post-meal sugar by 30% or more. That’s not magic—it’s biology. And it’s something you can do today, no prescription needed.
But diabetes management isn’t just about the numbers on a meter. It’s about avoiding the hidden dangers: nerve damage that makes your feet numb, kidney strain from high blood pressure, and eye problems that sneak up slowly. That’s why regular check-ups with your doctor aren’t optional—they’re your early warning system. And when you’re on multiple meds, like an ACE inhibitor for blood pressure and a statin for cholesterol, you need to watch for interactions. Some drugs can raise your sugar. Others can make your kidneys work harder. You don’t need to memorize every interaction, but you do need to ask: Could this new pill make my diabetes harder to control?
The good news? You’re not alone. Millions of people manage diabetes successfully every day—not perfectly, but consistently. They use apps to log meals, set phone alarms for meds, and talk to others in online groups. They learn that a bad day doesn’t ruin everything. What matters is getting back on track. And whether you’re just starting out or have been managing this for years, the tools and knowledge are out there. Below, you’ll find real advice from people who’ve been there: how to handle generic meds safely, what to do when your sugar won’t budge, how to spot warning signs before they become emergencies, and which supplements actually help—or hurt.
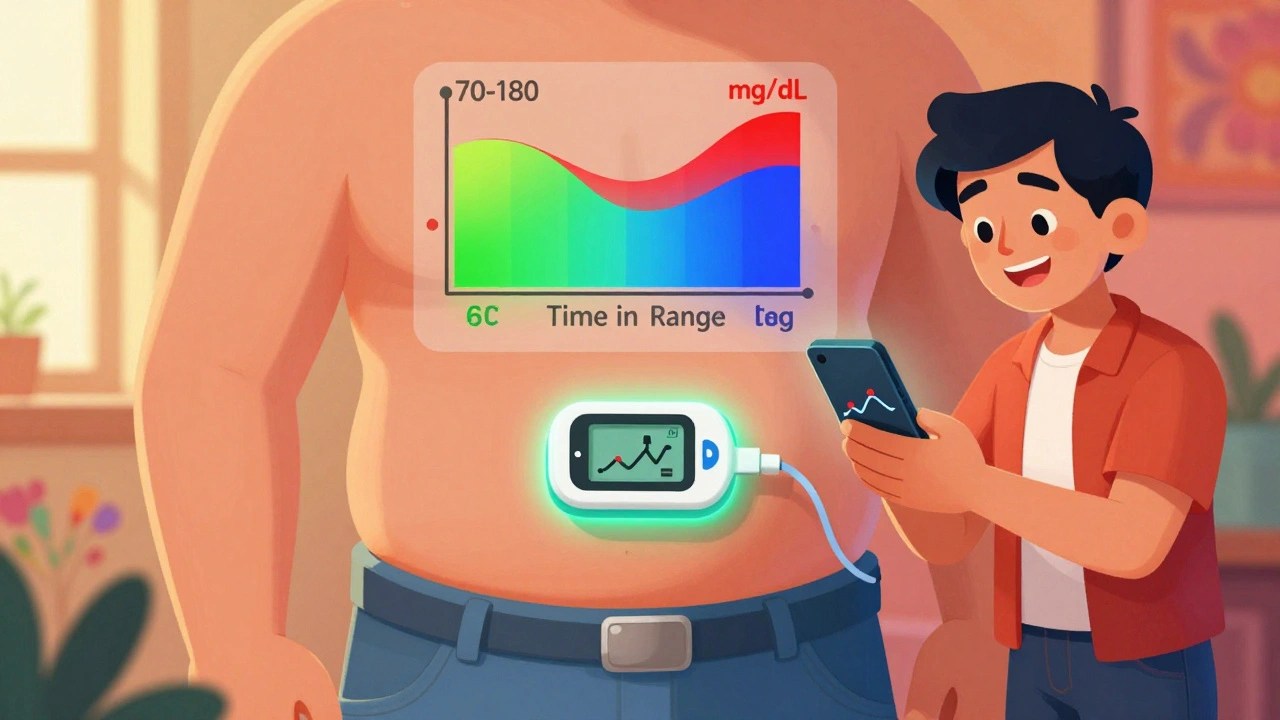
Time in Range: How CGM Metrics Help You Manage Diabetes Daily
Time in Range (TIR) uses continuous glucose monitoring to show how often your blood sugar stays in a healthy zone - giving you real-time control over diabetes, beyond what HbA1c can tell you.
- Dec 4, 2025
- Connor Back
- 8