CGM Metrics: What They Are, Why They Matter, and How They Guide Diabetes Care
When you hear CGM metrics, real-time data from a continuous glucose monitor that tracks your blood sugar levels every few minutes. Also known as glucose trends, these numbers don’t just show where your blood sugar is right now—they reveal how it moves, dips, and spikes over hours and days. This isn’t just for people with type 1 diabetes. More and more with type 2, prediabetes, or even those managing insulin resistance are using CGMs to understand how food, sleep, stress, and activity affect their bodies.
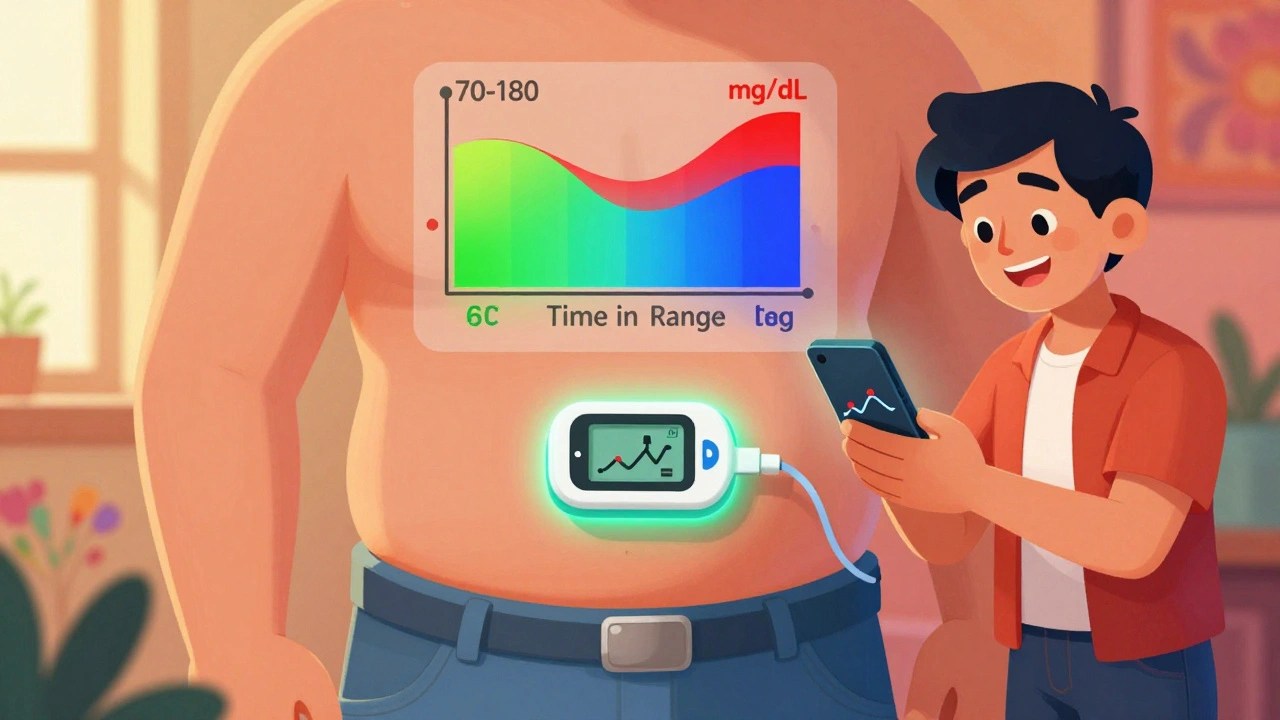
CGM metrics include things like time in range, the percentage of hours your glucose stays between 70 and 180 mg/dL, which is the gold standard for good control. Then there’s glucose variability, how much your numbers bounce up and down—high variability means more stress on your body, even if your average looks okay. You’ll also see hypoglycemia events, low blood sugar episodes that can happen without warning, and post-meal spikes, how high your sugar climbs after eating. These aren’t just numbers on a screen—they’re clues to what’s working and what’s not.
Unlike fingersticks that give you a single snapshot, CGM metrics show you the whole story. You might think your morning sugar is fine, but the trend line tells you it’s been climbing since 3 a.m. Or maybe your afternoon crash isn’t because you skipped lunch—it’s because your lunch had hidden carbs. That’s the power of continuous data. People who use CGM metrics regularly report fewer highs and lows, less guesswork, and more confidence in their daily choices. They adjust meals, timing, and activity based on real patterns, not luck.
And it’s not just about the numbers. The real win is how CGM metrics help you connect the dots between your life and your body. A night out with wine? A bad night’s sleep? A new workout routine? The device shows you the effect—no guesswork needed. That’s why doctors are pushing CGMs beyond type 1 diabetes. Even people on metformin or GLP-1 agonists are using them to fine-tune their treatment. It turns abstract advice like "eat less sugar" into concrete, personalized feedback.
What you’ll find below are real stories and practical guides from people who’ve used CGM metrics to take control. Some learned how to stop nighttime lows. Others found out their "healthy" granola bar spiked them like soda. One person cut their A1c by 2 points just by shifting meal timing after seeing their post-dinner trends. These aren’t theory pieces—they’re lived experiences, backed by data. Whether you’re new to CGMs or you’ve been using one for years, the posts here will help you read your numbers better, avoid common mistakes, and turn metrics into real change.
Time in Range: How CGM Metrics Help You Manage Diabetes Daily
Time in Range (TIR) uses continuous glucose monitoring to show how often your blood sugar stays in a healthy zone - giving you real-time control over diabetes, beyond what HbA1c can tell you.
- Dec 4, 2025
- Connor Back
- 8