Allergy Management in Cystic Fibrosis
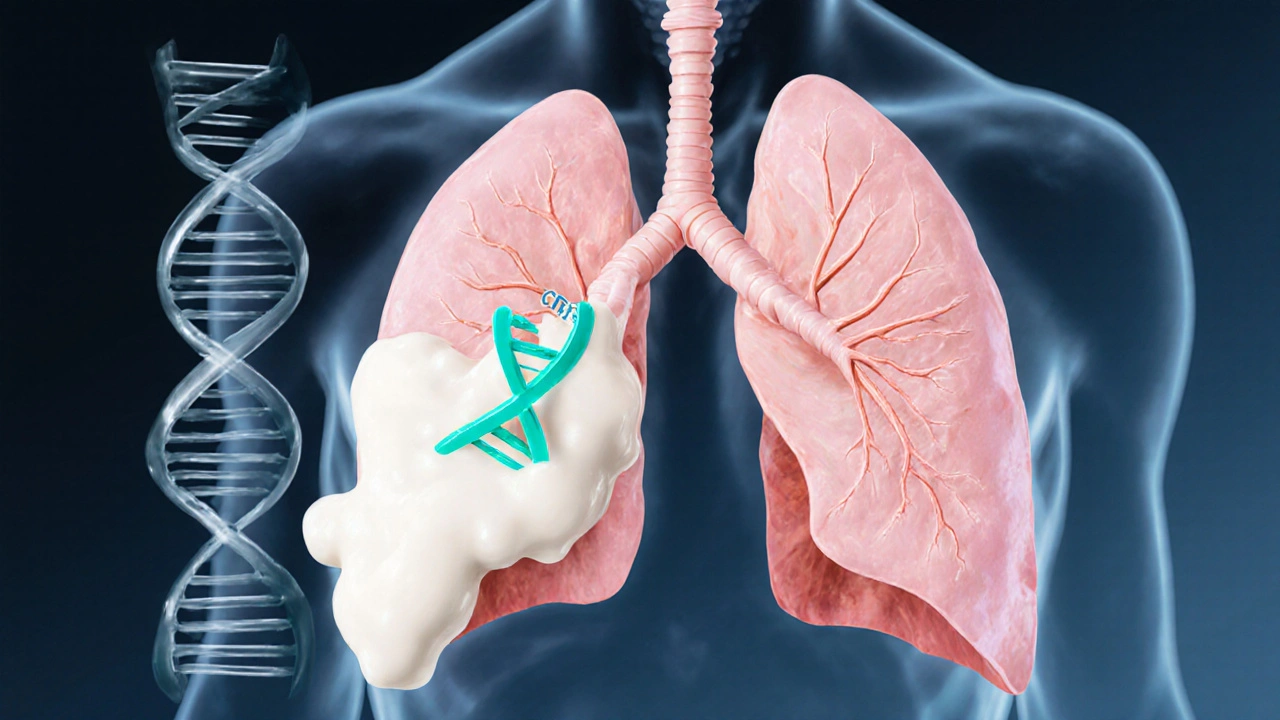
When dealing with allergy management in cystic fibrosis, the process of controlling allergic triggers and symptoms in people who have cystic fibrosis. Also known as CF allergy care, it is a cornerstone of maintaining good lung function.
People with cystic fibrosis, a genetic disorder that produces thick mucus in the lungs and digestive system often face heightened allergic reactions because their airways are already sensitive. Allergy, the immune system’s overreaction to harmless substances like pollen or dust can quickly turn into a respiratory flare‑up. That’s why respiratory therapy, techniques and treatments that keep the airways clear and reduce inflammation becomes essential. In short, effective allergy management requires a blend of trigger avoidance, medication, and targeted breathing exercises. It also means coordinating with a multidisciplinary team—doctors, physiotherapists, and pharmacists—so every aspect of care works together.
Key Strategies for Controlling Allergens
First, identify the most common triggers for CF patients: pollen, mold, pet dander, and indoor dust. A simple daily checklist can help spot patterns between exposure and symptom spikes. allergy management cystic fibrosis also benefits from regular indoor air quality checks; using HEPA filters and keeping humidity below 50 % reduces mold growth. Second, medication plays a big role. Antihistamines, nasal steroids, and leukotriene modifiers are often prescribed, but dosage must be adjusted for the higher mucus load in CF lungs. Third, integrate airway clearance techniques—flutter devices, chest physiotherapy, or high‑frequency chest wall oscillation—right after allergy medication to prevent mucus plugging. Finally, keep an emergency plan on hand: inhalers, rescue meds, and clear instructions for caregivers. When an allergy flare‑up triggers wheezing or shortness of breath, early intervention can stop a cascade that leads to an infection.
Beyond the basics, many CF patients find that regular exercise improves both allergy tolerance and overall lung capacity. Indoor workouts during high‑pollen seasons, such as yoga or stationary cycling, keep the heart rate up without exposing sensitive airways to outdoor allergens. Combining exercise with post‑session airway clearance maximizes the benefit. Nutrition also matters; omega‑3 rich foods and probiotics have shown promise in reducing inflammation linked to allergic responses. All of these pieces—environmental control, tailored medication, respiratory therapy, exercise, and diet—form a comprehensive approach that empowers patients to live with fewer allergy‑related setbacks.
Below you’ll see a curated list of articles that dive deeper into each of these areas. From step‑by‑step exercise plans for year‑round allergy sufferers to practical guides on buying affordable generic medicines, the collection gives you actionable insights you can start using today.
Cystic Fibrosis & Allergies: How They're Connected
Explore how cystic fibrosis and allergies intersect, learn the biological link, spot common allergy types, and get practical tips for managing both conditions safely.
- Oct 6, 2025
- Connor Back
- 20