CF Allergy Symptom Checker
People with cystic fibrosis are more prone to certain allergies due to chronic inflammation and thick mucus buildup. Here are the most frequently reported types:
- Allergic rhinitis (hay fever)
- Asthma-like airway hyper-reactivity
- Food allergies
- Atopic dermatitis (eczema)
- Sinusitis linked to allergens
Select symptoms you've experienced recently to see how they relate to cystic fibrosis and allergies:
Ever wondered why people with cystic fibrosis allergies seem to sneeze more or develop skin rashes? You’re not alone. Below we untangle the science, spot the warning signs, and give you practical steps to keep both conditions under control.
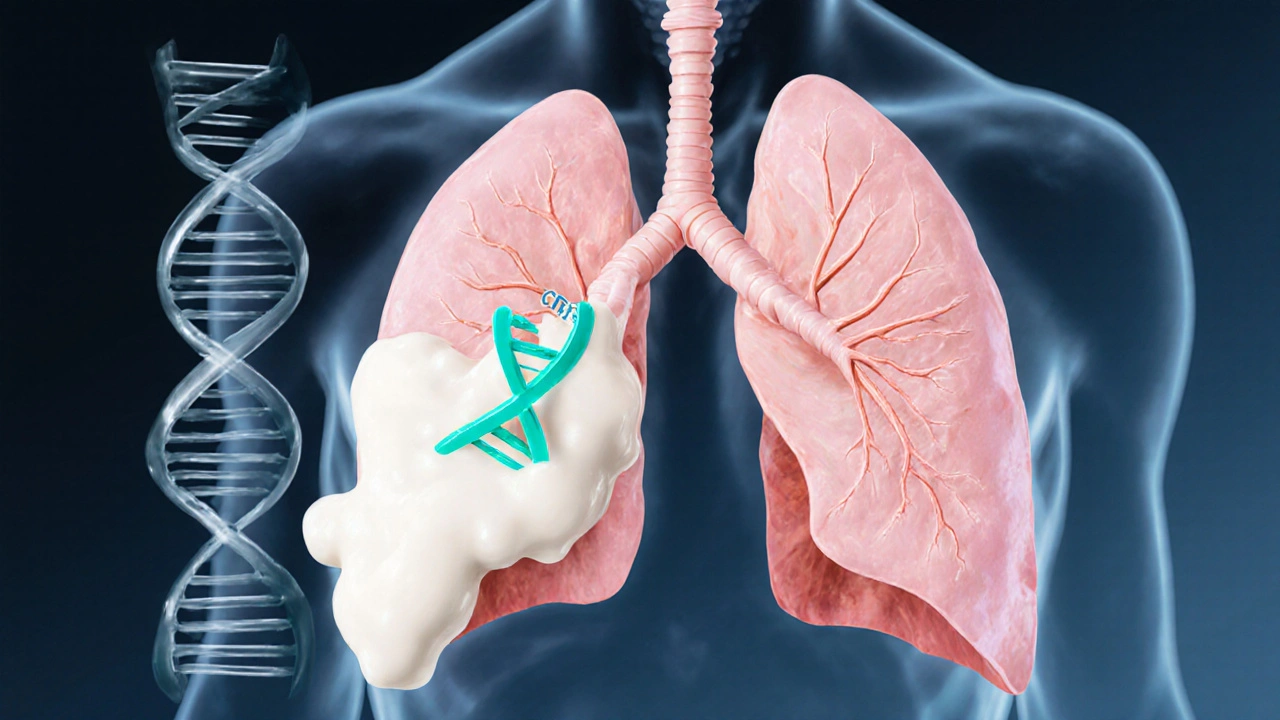
What is Cystic Fibrosis?
Cystic Fibrosis is a genetic disorder caused by mutations in the CFTR gene, which regulates the movement of salt and water across cell membranes. When the CFTR protein doesn’t work properly, thick mucus builds up in the lungs, pancreas, and other organs, leading to chronic infections and digestive problems. More than 70,000 people worldwide live with the condition, and the disease shows up differently from person to person.
How the Immune System Plays a Role in CF
The immune system in CF patients is constantly on high alert. The thick mucus traps bacteria, prompting relentless inflammation. Over time, this chronic inflammation can tilt the immune balance, making the body more likely to over‑react to harmless substances - that’s the classic allergy response.
Immune system functions as a network of cells and proteins that protect us from infections. In cystic fibrosis, the immune cells - especially neutrophils - are recruited in large numbers, releasing enzymes that damage lung tissue and also amplify allergic pathways.
Allergy Types That Show Up Frequently in CF
Allergies aren’t a one‑size‑fits‑all. Here’s a quick look at the ones most often reported by people with cystic fibrosis:
| Allergy Type | Typical Symptoms | Prevalence in CF (%) | Management Tip |
|---|---|---|---|
| Allergic rhinitis (hay fever) | Sneezing, runny nose, itchy eyes | 30-45 | saline rinses + antihistamine safe with CF meds |
| Asthma‑like airway hyper‑reactivity | Wheezing, chest tightness, shortness of breath | 25-35 | Inhaled corticosteroids, monitor lung function regularly |
| Food allergy (e.g., nuts, shellfish) | Hives, stomach cramps, anaphylaxis (rare) | 10-15 | Avoid trigger, carry epinephrine if severe |
| Atopic dermatitis (eczema) | Dry, itchy skin patches | 20-30 | Moisturize often, low‑potency topical steroids |
| Sinusitis linked to allergens | Facial pain, thick nasal discharge, worsened cough | 40-55 | Nasal steroids, consider allergy testing |
The Biological Link: CFTR, IgE, and Inflammation
Scientists have uncovered a few key mechanisms that explain why allergy rates are higher in CF:
- CFTR dysfunction leads to altered ion transport in airway epithelial cells, which can increase the release of cytokines that attract IgE‑producing B cells. High IgE levels are a hallmark of allergic reactions.
- Chronic bacterial colonisation (often Pseudomonas aeruginosa) keeps the immune system in a pro‑inflammatory state, lowering the threshold for an allergic flare.
- Sticky mucus hampers the clearance of allergens from the nasal passages and lungs, giving them more time to interact with immune cells.
In short, a broken CFTR gate, persistent infection, and thick mucus together create a perfect storm for allergies.
How Allergies Impact Overall CF Health
Allergies aren’t just annoying; they can worsen the core problems of cystic fibrosis:
- Airway obstruction: Nasal congestion and post‑nasal drip increase mucus production, making it harder to clear the lungs.
- Exacerbations: An allergic flare can mimic or trigger a pulmonary exacerbation, leading to extra antibiotics and hospital visits.
- Nutritional issues: Food allergies limit dietary options, which is already a challenge with pancreatic insufficiency.
- Quality of life: Persistent itching, sneezing, or sinus pain adds to the daily treatment burden.
Managing Allergies When You Have Cystic Fibrosis
Effective allergy control starts with a clear picture of what’s bothering you. Here’s a step‑by‑step plan that works for most CF families:
- Get tested: An allergist can perform skin‑prick or serum IgE tests. Knowing the exact triggers lets you avoid unnecessary exposures.
- Environmental control: Use HEPA filters, wash bedding in hot water weekly, and keep indoor humidity low to limit mold spores.
- Medication coordination: Many antihistamines (e.g., loratadine) are safe with CF antibiotics. Discuss any new drug with your pulmonologist to avoid interactions.
- Consider immunotherapy: For persistent allergic rhinitis or asthma, allergy shots or sublingual tablets can desensitize the immune system. Recent studies show they do not worsen lung function in CF patients.
- Integrate with airway therapy: Daily chest physiotherapy plus nasal saline rinses can clear both mucus and allergens simultaneously.
Never stop a prescribed CF medication to treat an allergy - always add, never subtract, without professional guidance.

When to Call Your Healthcare Team
Some red‑flag signs mean you should seek help right away:
- Sudden drop in lung function (FEV1 falls >10%).
- Persistent high‑fever or new sputum colour.
- Severe skin reaction spreading quickly.
- Shortness of breath that doesn’t improve with rescue inhaler.
Prompt consultation can prevent an allergy from turning into a dangerous CF exacerbation.
Quick Takeaways
- CF patients are predisposed to several types of allergies because of chronic inflammation and mucus buildup.
- Allergies can worsen lung function, increase infection risk, and affect nutrition.
- Identify triggers through testing, control the environment, and coordinate allergy meds with CF therapies.
- Immunotherapy is a safe option for many, but always discuss with both an allergist and CF specialist.
- Watch for rapid symptom changes and seek medical help early.
Frequently Asked Questions
Can I take over‑the‑counter antihistamines with my CF medications?
Most second‑generation antihistamines (like cetirizine or loratadine) do not interact with common CF antibiotics or mucolytics. Still, check with your pharmacist because some cough suppressants can affect airway clearance.
Is allergy testing safe for people with cystic fibrosis?
Yes. Skin‑prick tests and specific IgE blood tests are routine and well‑tolerated. The only precaution is to avoid performing tests during an active pulmonary exacerbation.
Do allergies increase the risk of lung infections in CF?
Allergic inflammation can thicken mucus, making it a better breeding ground for bacteria like Pseudomonas. Managing allergies therefore helps lower infection risk.
Can I get allergy shots if I have cystic fibrosis?
Allergy immunotherapy is considered safe for most CF patients. It should be done under a specialist who monitors lung function, because any systemic reaction could affect breathing.
What lifestyle changes help both CF and allergies?
Regular airway clearance, a low‑sodium diet, staying hydrated, using HEPA‑filtered air, and keeping the home free of pets or dust mites can reduce both mucus buildup and allergic reactions.

Written by Connor Back
View all posts by: Connor Back