Drug Interaction Checker: Statins & Antifungals
Check Your Medication Combination
When you’re taking a statin to lower your cholesterol and then get a serious fungal infection, things can get dangerous fast. Systemic antifungals-especially the azole class-are lifesavers for deep fungal infections, but they don’t play nice with statins or immunosuppressants. These combinations can push your muscle tissue into a breakdown state called rhabdomyolysis, which can lead to kidney failure or even death. And despite clear warnings, these risky pairings still happen more often than they should.
Why Azole Antifungals Are So Risky with Statins
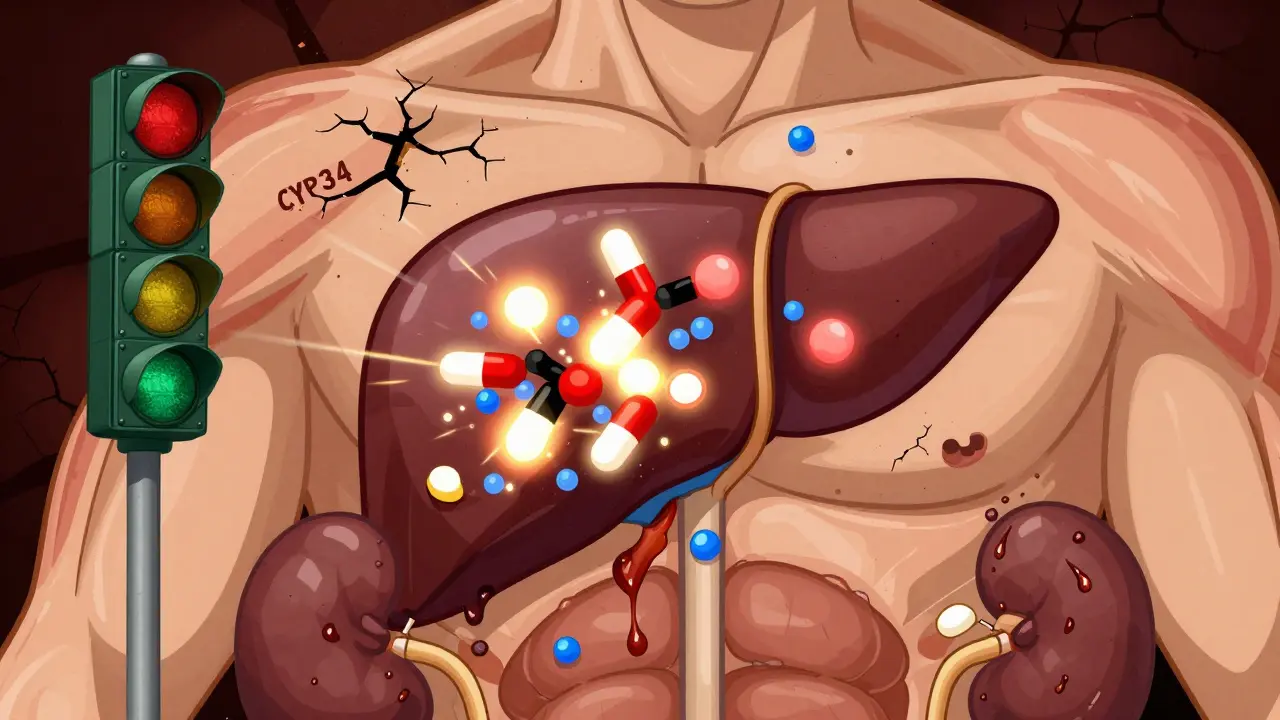
Azole antifungals like fluconazole, itraconazole, voriconazole, posaconazole, and ketoconazole work by blocking a fungal enzyme called lanosterol 14-alpha-demethylase. But here’s the catch: that same enzyme exists in humans as part of the CYP3A4 liver system. CYP3A4 breaks down about 30% of all prescription drugs, including most statins. When azoles block it, statins build up in your blood like traffic on a highway with no exits. The biggest culprits? Ketoconazole and posaconazole. These are strong CYP3A4 inhibitors. When taken with simvastatin or lovastatin, they can spike statin levels by 15 to 20 times. Even atorvastatin, the most commonly prescribed statin, can jump 10-fold. That’s not a minor bump-it’s a red alert. The result? Muscle pain, weakness, dark urine, and in severe cases, rhabdomyolysis. One study found that patients on both an azole and a CYP3A4-metabolized statin had a tenfold higher risk of muscle damage than those on statins alone. Not all statins are created equal. Pravastatin and rosuvastatin don’t rely heavily on CYP3A4, so they’re safer choices. But even they aren’t risk-free. Ketoconazole also blocks the OATP1B1 transporter, which helps move statins out of the liver. That means pravastatin and rosuvastatin can still pile up if ketoconazole is in the mix. Fluconazole is less risky than ketoconazole, but it still messes with CYP2C9 and CYP2C19, which can affect other drugs you might be taking.Immunosuppressants Make It Even Worse
If you’ve had a kidney, liver, or heart transplant, you’re probably on cyclosporine, tacrolimus, or sirolimus. These drugs keep your immune system from rejecting the new organ-but they also block CYP3A4 and P-glycoprotein, the same systems statins depend on to get cleared from your body. In transplant patients, combining statins with cyclosporine can increase statin levels by 3 to 20 times. That’s why up to 25% of transplant recipients on statins develop muscle symptoms. And when creatine kinase (CK) levels climb past 10,000 U/L, you’re looking at full-blown rhabdomyolysis. One case report described a patient whose CK hit 24,000 U/L after starting fluconazole while on simvastatin and cyclosporine. He ended up in the ICU. The problem isn’t just one drug. It’s the combo. Many transplant patients need both an immunosuppressant and a statin to manage high cholesterol, which is common after transplant due to steroid use. But doctors often don’t realize how dangerous this mix is until it’s too late.Which Statins Are Safe? Which Aren’t?
Here’s the simple breakdown:- AVOID: Simvastatin, lovastatin, atorvastatin-these are metabolized almost entirely by CYP3A4. Even a moderate dose can become toxic when paired with an azole.
- USE WITH CAUTION: Pravastatin and rosuvastatin-less dependent on CYP3A4, but still vulnerable to OATP1B1 inhibition by ketoconazole. Lower doses (pravastatin 10-20 mg, rosuvastatin 5-10 mg) are safer.
- SAFER OPTIONS: Fluvastatin and pitavastatin-mostly cleared by other liver enzymes, making them better choices if you need ongoing statin therapy during antifungal treatment.
And here’s a hard rule: if you’re on ketoconazole or posaconazole, stop simvastatin, lovastatin, and atorvastatin entirely. Don’t just lower the dose-hold it. Wait until the antifungal is completely out of your system. Posaconazole sticks around for 24 to 30 hours after your last dose. Restarting your statin too soon can still cause trouble.

What Doctors Should Do-And What You Should Ask
Clinicians have clear guidelines from the American College of Cardiology and the Infectious Diseases Society of America:- Switch to pravastatin or rosuvastatin at the lowest effective dose.
- For high-risk patients, consider twice-weekly dosing instead of daily.
- Monitor creatine kinase levels before starting antifungals and weekly during treatment.
- If CK rises above 10 times the upper limit of normal, stop the statin immediately.
- Check immunosuppressant blood levels when starting or stopping azoles-trough levels may need to be cut by 30-50%.
But real-world practice lags behind guidelines. A 2012 study found that doctors still prescribe simvastatin with azoles far too often-even though the drug labels say not to. Why? Because it’s easy. Prescribing fluconazole for a yeast infection feels routine. Prescribing a statin for high cholesterol feels routine. No one stops to think about the interaction.
Electronic health records help. Hospitals with clinical decision support systems reduced dangerous combinations by 47%. But in community pharmacies and smaller clinics, those alerts are often turned off or ignored. That’s where you come in.
Ask your doctor: “Is this antifungal going to interact with my cholesterol pill?” Ask your pharmacist: “Do I need to stop my statin while taking this?” If they don’t know, ask for a pharmacist consult. You’re not being difficult-you’re protecting your muscles, your kidneys, and your life.
Newer Antifungals Offer Hope
There’s some good news. Newer antifungals are being designed to avoid these interactions. Isavuconazole, approved in 2015, is a moderate CYP3A4 inhibitor-less risky than ketoconazole. Olorofim, currently in phase 2 trials, doesn’t touch the CYP450 system at all. It works by blocking a completely different fungal enzyme, so it shouldn’t interfere with statins or immunosuppressants. Pharmacists in 87% of academic medical centers now use a mandatory verification protocol before dispensing azoles to patients on statins. That’s cut dangerous prescriptions by 63%. It’s not perfect, but it’s progress.
Genetic Risk: Are You More Vulnerable?
Some people are naturally at higher risk. About 12% of the population has a gene variant called SLCO1B1*5. This mutation reduces the liver’s ability to take up statins, causing them to build up even without drug interactions. If you have this variant and take a statin with an azole, your risk of muscle damage skyrockets. Right now, genetic testing isn’t routine. But if you’ve had unexplained muscle pain on statins before, or if you’re a transplant patient who’s had muscle issues, it’s worth asking your doctor about testing. Knowing your genetic risk could change your treatment plan forever.Bottom Line: Don’t Guess. Check.
Systemic antifungals are powerful. Statins save lives. Immunosuppressants keep transplants alive. But together? They can destroy muscle tissue. The risk isn’t theoretical-it’s documented, measured, and deadly. If you’re on a statin and need an antifungal:- Don’t assume your doctor knows the interaction.
- Don’t take your statin unless you’re told it’s safe.
- Don’t restart your statin without checking with your provider after the antifungal ends.
- Report muscle pain, weakness, or dark urine immediately.
There’s no room for hesitation. A few days without your statin won’t ruin your cholesterol control. But one episode of rhabdomyolysis could end your life.
Can I take fluconazole with my statin?
Fluconazole is a moderate CYP3A4 inhibitor and can raise levels of atorvastatin, simvastatin, and lovastatin. It’s safer than ketoconazole or posaconazole, but still risky. The best choice is to switch to pravastatin or rosuvastatin at a reduced dose. If you must keep your current statin, your doctor should lower the dose significantly and monitor you closely.
What if I’m on cyclosporine after a transplant?
Combining cyclosporine with any statin increases the risk of muscle damage by 3 to 20 times. Pravastatin or rosuvastatin at the lowest effective dose is preferred. Avoid simvastatin and lovastatin entirely. Your transplant team should monitor your creatine kinase and cyclosporine blood levels every week during antifungal treatment.
How long should I wait to restart my statin after stopping an azole?
It depends on the antifungal. For fluconazole, wait 2-3 days. For itraconazole or voriconazole, wait 5-7 days. For posaconazole, wait at least 7 days-its half-life is 24-30 hours, so it lingers in your system. Always confirm with your doctor before restarting. Never assume it’s safe just because you’re done taking the antifungal.
Is there a statin that’s completely safe with antifungals?
No statin is 100% safe with all antifungals, but fluvastatin and pitavastatin are the least likely to interact because they’re metabolized by enzymes other than CYP3A4. Pravastatin and rosuvastatin are next best, but still require caution with ketoconazole due to OATP1B1 inhibition. Always use the lowest effective dose.
What symptoms should I watch for?
Watch for unexplained muscle pain, tenderness, or weakness-especially in your shoulders, thighs, or lower back. Dark or cola-colored urine is a red flag. Fatigue, nausea, or fever can also signal trouble. If you notice any of these, stop your statin and call your doctor immediately. Don’t wait. Rhabdomyolysis can damage your kidneys within hours.

Written by Connor Back
View all posts by: Connor Back