When you start taking a statin to lower your cholesterol, you expect to feel better - not worse. But for a lot of people, muscle pain, stiffness, or weakness shows up soon after. It’s not just "old age" or "too much gym." It’s real. And it’s common enough that doctors now have a name for it: statin intolerance. The problem isn’t that statins are dangerous - they’re not. It’s that many people stop taking them because of symptoms that might not even be caused by the drug. And when they stop, their heart risk goes up. That’s the real danger.
What Exactly Is Statin Intolerance?
Statin intolerance isn’t just "I feel sore." It’s a specific clinical diagnosis. According to the National Lipid Association (2022), you’re considered statin-intolerant only if you can’t take two different statins: one at the lowest dose, and another at any dose - because of symptoms that go away when you stop the drug. That’s the gold standard. Too many people get labeled as intolerant after trying just one statin, and that’s wrong. In fact, 65% of people who can’t handle one statin can tolerate another just fine.
The real issue? Most muscle symptoms aren’t from statins at all. The SAMSON trial showed that 90% of patients reported muscle pain even when they were taking a sugar pill instead of a statin. That’s the nocebo effect - your brain expecting side effects, so you feel them. A study of over 1,200 patients found that 78% blamed statins for aches before even seeing a doctor. Later, many found other causes: arthritis, vitamin D deficiency, or just normal wear and tear.
Where Do the Symptoms Show Up?
If you’re truly experiencing statin-associated muscle symptoms (SAMS), they usually hit the big muscles: thighs (78% of cases), buttocks (65%), back (52%), and shoulders (47%). You don’t get sharp pain. You get heaviness (62%), stiffness (57%), or cramps (49%). It’s not a pulled muscle. It’s more like your legs feel like they’re wrapped in concrete. Some people can’t get up from a chair without using their arms. Others can’t lift their hands over their head. These aren’t random complaints - they’re documented patterns from large studies.
Here’s what’s surprising: 89% of people with these symptoms have normal or only slightly raised creatine kinase (CK) levels. That’s the enzyme doctors check for muscle damage. If your CK is more than 10 times normal, you might have real muscle injury - myositis. If it’s over 40 times normal with dark urine, you’re at risk for rhabdomyolysis. But those are extremely rare. The FDA says only about 300-500 cases of rhabdomyolysis happen each year among 200 million statin users. So most muscle pain? Not a medical emergency. Just a nuisance.
Why Do Some People Have It and Others Don’t?
It’s not random. Genetics play a role. Some people carry a variant in the SLCO1B1 gene - especially the *5 or *15 alleles - that makes it harder for their body to clear statins. That raises muscle symptom risk by 4.5 times. That’s why by 2025, the European Atherosclerosis Society expects 30% of new statin users to get genetic testing before starting. It’s not mainstream yet, but it’s coming.
Drug interactions matter too. If you’re on a statin and also taking something that blocks the liver enzyme CYP3A4 - like certain antibiotics, antifungals, or grapefruit juice - your statin builds up. That raises your risk. About 22% of people with statin symptoms are on one of these interacting drugs. And if you’re low on vitamin D (29% of cases), or have an underactive thyroid (12%), your muscles are already stressed. Fix those first.
What’s the Best Way to Confirm It’s Statin-Related?
Doctors need to do three things to get it right:
- Stop the statin for 2-4 weeks. Do symptoms go away?
- Rule out other causes - thyroid, vitamin D, arthritis, fibromyalgia.
- Re-challenge: Try the same statin again. If symptoms come back, you might be truly intolerant. If they don’t? You were never intolerant.
Only 34% of people who think they’re intolerant actually have symptoms return on re-challenge. That means over two-thirds of people who quit statins could have stayed on them. That’s a huge missed opportunity for heart protection.
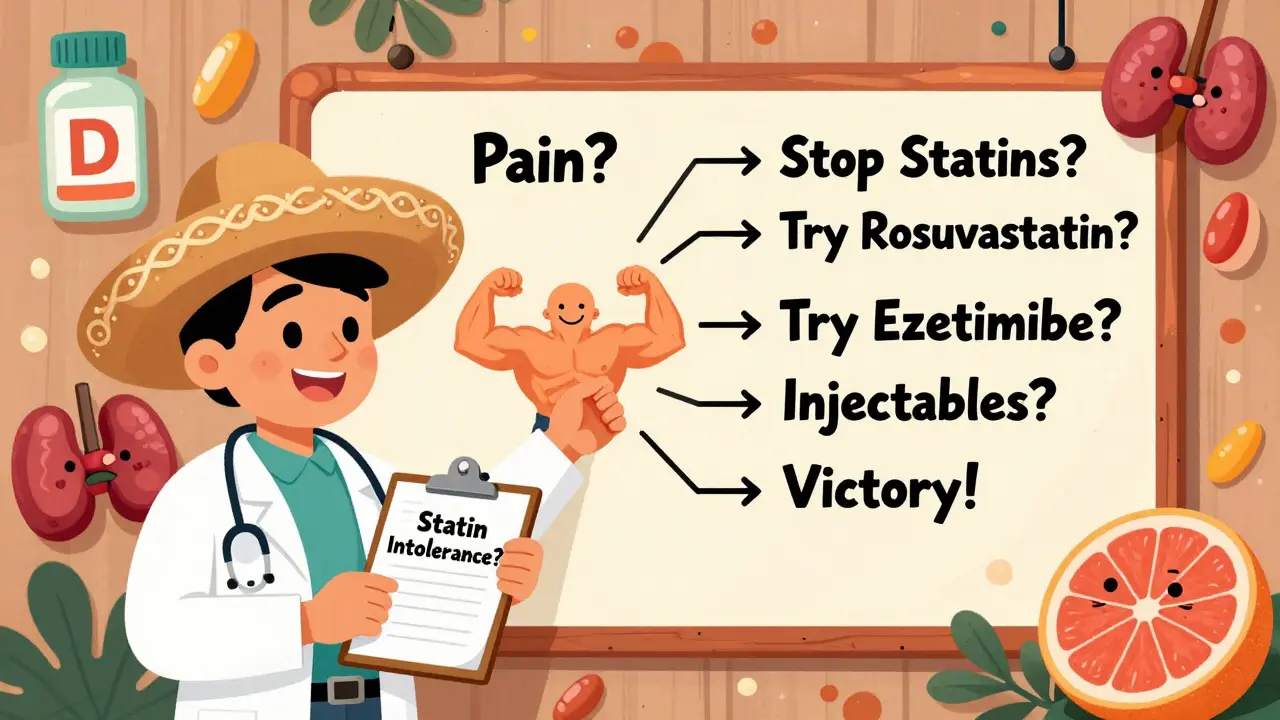
What Are Your Alternatives If You Really Can’t Tolerate Statins?
Here’s the good news: You don’t have to give up on lowering your cholesterol. There are effective, well-tested options.
1. Switch Statins
Not all statins are the same. Lipophilic statins - like simvastatin and atorvastatin - cross into muscle tissue more easily. That’s why they’re linked to more symptoms. Hydrophilic statins - pravastatin and rosuvastatin - stay mostly in the liver. Studies show they cause 28% fewer muscle problems. Try a low dose of rosuvastatin (5-10 mg) or pravastatin (20-40 mg). Many people switch and never look back.
2. Try Ezetimibe
Ezetimibe (Zetia) blocks cholesterol absorption in your gut. It lowers LDL by about 18% on its own. It’s well tolerated - 94% of people stick with it after a year. It’s cheap, generic, and has almost no side effects. It’s not as powerful as a statin, but it’s a solid first step. Often, doctors pair it with a low-dose statin to get better results without high side effects.
3. Bempedoic Acid (Nexletol)
This newer drug works in the liver, not the muscle. It lowers LDL by 17% and has been shown to reduce heart attacks and strokes in high-risk patients. It’s taken as a pill once a day. Tolerability is high - 88% of people stay on it. It’s not perfect (some get tendon issues or elevated uric acid), but for those who can’t touch statins, it’s a game-changer.
4. PCSK9 Inhibitors (Repatha, Praluent)
These are injectables - once every two weeks. They drop LDL by nearly 60%. They’re not first-line because they’re expensive ($5,800/year), but insurance often covers them if you’ve tried and failed other options. In the SPIRE-1 trial, 91% of patients stayed on the treatment. They’re especially useful for people with genetic high cholesterol or those with diabetes and heart disease.
5. Inclisiran (Leqvio)
This is the future. It’s an RNA-based therapy given as just two shots a year. It lowers LDL by 50% and works by silencing the gene that makes PCSK9. In trials, 93% of people stayed on it. It’s not yet widely available, but it’s approved in the U.S. and Europe. If you hate pills or shots, this might be the best long-term option.

What About CoQ10 or Other Supplements?
Many people try CoQ10 because statins lower CoQ10 levels in the body. The theory makes sense. But double-blind studies show only 34% of people report feeling better. That’s not much better than placebo. Vitamin D? If you’re deficient, yes - fix it. But taking extra CoQ10 just because you’re on a statin? Don’t count on it.
What Happens If You Just Quit?
Here’s the hard truth: 45-60% of statin prescriptions are stopped within a year. Muscle pain is the top reason. But stopping statins without replacing them increases your risk of heart attack or stroke by 25%. The cost? About $1,800 more per person per year in medical bills. That’s not just numbers - that’s someone ending up in the ER, needing stents, or worse.
Patients who quit often feel anxious. One Reddit user wrote: "I stopped statins because my legs hurt. Now I’m scared I’m going to die of a heart attack." That fear is real. But the solution isn’t avoiding meds - it’s finding the right ones.
What’s the Bottom Line?
Statin intolerance is often misunderstood. Most muscle pain isn’t caused by statins. Most people who think they’re intolerant can actually take a different statin. And if they truly can’t, there are effective alternatives - from ezetimibe to inclisiran. The key is not quitting. It’s working with your doctor to find the right path.
Don’t assume your muscle pain is from statins. Get tested. Rule out other causes. Try a different statin. Use ezetimibe. Consider bempedoic acid or injectables if needed. You don’t have to live with high cholesterol. And you don’t have to live with pain. There’s a way forward - if you don’t give up.
Can statins cause permanent muscle damage?
No. Statin-related muscle symptoms are almost always reversible. Once you stop the drug, symptoms fade within days to weeks. True muscle damage - like myositis or rhabdomyolysis - is extremely rare, and even then, recovery is common with proper care. There’s no evidence that statins cause lasting harm to muscles in the vast majority of cases.
Is it safe to take statins every other day or once a week?
Yes, for some people. Intermittent dosing - like 600 mg of rosuvastatin once a week - can lower LDL by nearly 50% in those who can’t tolerate daily dosing. It’s not for everyone, but studies show it works for about two-thirds of patients who’ve tried it. This approach reduces exposure to the drug while keeping cholesterol under control. Always do this under a doctor’s supervision.
Why do some doctors still say statins are safe even if I feel bad?
Because the data shows statins cause muscle symptoms in only about 5 out of every 1,000 patients per year - almost the same rate as placebo. Doctors aren’t dismissing your pain. They’re trying to figure out if it’s really from the statin or something else - like arthritis, vitamin deficiency, or the nocebo effect. The goal is to keep you protected from heart disease without unnecessary suffering.
Are non-statin cholesterol drugs as effective as statins?
Some are. PCSK9 inhibitors like evolocumab lower LDL by 59%, which is stronger than most statins. Bempedoic acid and ezetimibe are weaker - around 15-18% reduction - but still meaningful. They’re not "as good" as high-dose statins, but they’re good enough for many people. The key is matching the drug to your risk. For someone with a history of heart attack, a PCSK9 inhibitor may be the best choice. For someone with mild risk, ezetimibe may be enough.
How long does it take to find the right alternative therapy?
Usually 3 to 6 months. Finding the right combination often takes trial and error. You might try switching statins, then add ezetimibe, then move to bempedoic acid. Real-world data shows patients try an average of 2.3 different strategies before hitting their LDL goal. Patience and persistence matter. Don’t give up after one failed attempt.


Written by Guy Boertje
View all posts by: Guy Boertje