PPI Selection Guide for Antiplatelet Therapy
Select your current dual antiplatelet therapy regimen:
Critical Safety Note:
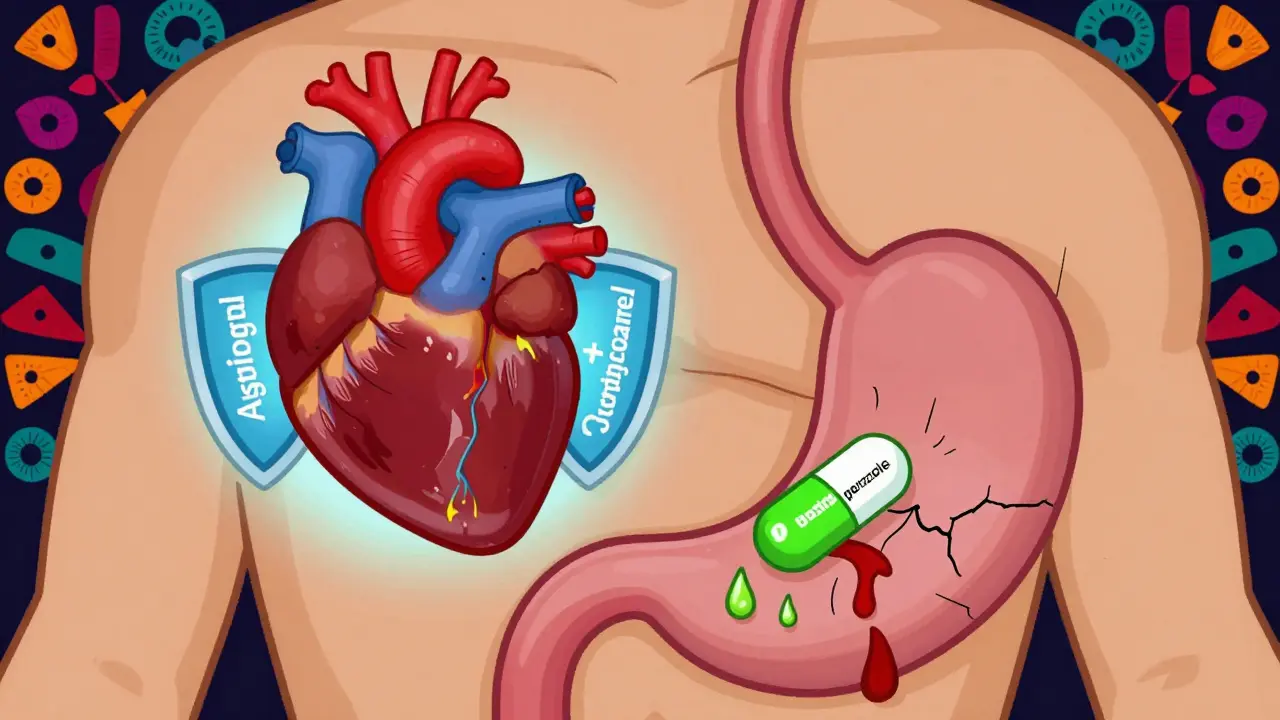
Do NOT use omeprazole with clopidogrel as it reduces heart protection by 30-45%.
When you’re on dual antiplatelet therapy - usually aspirin plus clopidogrel, prasugrel, or ticagrelor - your blood doesn’t clot as easily. That’s good for preventing heart attacks and strokes. But it also means your stomach is more vulnerable. Up to 50% of people on this combo develop gastrointestinal (GI) bleeding within the first year, especially if they’re over 65, have had a past ulcer, or take NSAIDs like ibuprofen. The fix? Proton pump inhibitors (PPIs). But not all PPIs are created equal. Choosing the wrong one can undo the heart benefits you’re trying to protect.
Why GI Bleeding Is a Real Threat on Antiplatelets
Aspirin and other antiplatelet drugs don’t just thin your blood - they also damage the lining of your stomach and upper intestines. The acid in your stomach, which normally helps digest food, starts eating away at the unprotected tissue. The result? Bleeding, ulcers, even life-threatening blood loss. Studies show that people on dual antiplatelet therapy have a 30-50% higher risk of GI bleeding compared to those on aspirin alone. And half of those bleeds happen in the first 30 days after starting treatment.It’s not just about being older. If you’ve had a previous ulcer, take steroids, use NSAIDs, or are on blood thinners like warfarin, your risk shoots up. Yet, many patients - and even some doctors - don’t realize how quickly this can happen. A 2025 Korean study of nearly 97,000 stroke patients on dual therapy found that 325 major GI bleeds occurred over 12 months. That’s not rare. It’s predictable. And it’s preventable.
How PPIs Work - And Why They’re Essential
Proton pump inhibitors block the final step of acid production in your stomach. They don’t just reduce acid - they shut it down by 70-98%, depending on the drug and dose. This lets the stomach lining heal and prevents new ulcers from forming. Multiple large studies, including the landmark COGENT trial published in JAMA in 2010, show that adding a PPI cuts major GI bleeding by 34-37%. That’s not a small benefit. It’s life-saving.Here’s the catch: not every PPI plays nice with your antiplatelet drugs. The problem centers on a liver enzyme called CYP2C19. It’s how your body activates clopidogrel. If a PPI blocks this enzyme, clopidogrel can’t do its job - and your risk of heart attack or stroke goes up.
Which PPI Is Safe With Clopidogrel? Not All Are Equal
If you’re on clopidogrel, omeprazole is a bad choice. It cuts clopidogrel’s effectiveness by 30-45%. That’s not theoretical. A 2010 meta-analysis in Circulation found a 27% higher risk of cardiovascular events in patients taking omeprazole with clopidogrel.But pantoprazole and esomeprazole? They barely touch CYP2C19. Studies show less than a 15% reduction in clopidogrel’s antiplatelet effect - clinically insignificant. That’s why guidelines now recommend them as first-line choices when clopidogrel is part of your regimen.
Here’s what works:
- Pantoprazole 40 mg daily - Best for clopidogrel users. Minimal interaction, strong protection.
- Esomeprazole 40 mg daily - Also safe with clopidogrel. Even better if you’re on ticagrelor or prasugrel - neither of which rely on CYP2C19.
- Omeprazole - Avoid if on clopidogrel. Use only if no alternatives exist and you’re not on clopidogrel.
And don’t confuse PPIs with H2 blockers like famotidine. They’re weaker. A 2017 meta-analysis in JAMA Internal Medicine found PPIs reduced GI bleeding by 60%, while H2 blockers only cut it by 30%. If you’re at risk, go with the stronger option.

Who Should Get a PPI - And Who Doesn’t Need One
Not everyone on antiplatelets needs a PPI. The key is risk. The 2023 European Society of Cardiology guidelines say: give a PPI if you have two or more of these:- Age 65 or older
- History of GI bleeding or ulcer
- Taking NSAIDs (ibuprofen, naproxen)
- Using corticosteroids
- On anticoagulants (like warfarin or apixaban)
That’s it. If you’re 50, healthy, no past ulcers, no other meds - you probably don’t need it. And here’s the scary part: 35-45% of PPI prescriptions in DAPT patients are unnecessary, according to a 2022 American Journal of Cardiology study. That’s overprescribing. And it comes with its own risks.
The Hidden Dangers of Taking PPIs Too Long
PPIs are safe for short-term use. But if you take them for years without reason, you’re exposing yourself to problems you didn’t sign up for:- Clostridium difficile infection - Risk increases by 0.5%. Not huge, but serious when it hits.
- Community-acquired pneumonia - Risk up by 0.8%.
- Chronic kidney disease - Long-term use linked to a 20% higher hazard ratio.
- Bone fractures - FDA has a black box warning for high-dose, long-term use.
And now, emerging data suggests a possible link to dementia - though a 2025 Mendelian randomization study in JAMA Internal Medicine found no causal link. The science isn’t settled. But what’s clear: don’t take a PPI longer than you need to.
For most people on dual antiplatelet therapy, 6-12 months is enough. After that, reassess. If you’re stable, off NSAIDs, no other risk factors - you can often stop safely.

What About Newer Drugs? Vonoprazan Is Coming
There’s hope on the horizon. A new class of acid blockers called potassium-competitive acid blockers (P-CABs) is in the pipeline. Vonoprazan, for example, works faster and stronger than PPIs - and doesn’t interfere with CYP2C19 at all. In the phase III VENOUS trial, it matched esomeprazole in preventing GI bleeding - without the drug interaction risk.The FDA is reviewing it as of Q3 2025. If approved, it could become the new gold standard - especially for patients on clopidogrel who need long-term protection. Until then, stick with pantoprazole or esomeprazole.
Practical Tips: How to Get It Right
If you’re on aspirin plus clopidogrel, prasugrel, or ticagrelor:- Start the PPI on day one - Most bleeds happen in the first 30 days.
- Use pantoprazole 40 mg daily if on clopidogrel. Use esomeprazole 40 mg if on ticagrelor or prasugrel.
- Don’t take omeprazole with clopidogrel - it’s a known risk.
- Review your meds every 6 months - Are you still on NSAIDs? Did your ulcer heal? Are you still at risk?
- Ask your doctor about stopping after 6-12 months - if your risk has dropped.
And if your doctor prescribes omeprazole with clopidogrel? Ask why. There’s almost always a better option.
Bottom Line: Protection Without Compromise
You need your antiplatelets to keep your heart and brain safe. You also need to keep your stomach from bleeding. The good news? You don’t have to choose. With the right PPI - pantoprazole or esomeprazole - you get both. The wrong PPI? You might trade one risk for another.It’s not about taking more pills. It’s about taking the right ones. And timing matters. Start early. Choose wisely. Stop when you can. That’s how you protect your whole body - not just your heart.

Written by Connor Back
View all posts by: Connor Back