Antidepressant Efficacy & Side Effect Tracker
How This Works
Track your symptoms using the PHQ-9 scale and side effects with the Antidepressant Side-Effect Checklist. We'll calculate your efficacy score versus side effect burden to help you understand if your treatment is working.
PHQ-9 Depression Tracker
Rate your symptoms over the past 2 weeks (0-3 scale)
Side Effect Tracker
Rate each side effect (0-4 scale)
Enter your scores to see your treatment balance
When you start an antidepressant, you’re not just taking a pill-you’re stepping into a long-term experiment with your own body and mind. The goal is simple: feel better. But what happens when the pill helps your mood but makes you feel numb, sleepy, or like your sex drive has vanished? Or worse-what if it doesn’t help at all? This isn’t rare. About 30-40% of people don’t get relief from their first antidepressant, and 74% deal with at least one side effect. The real question isn’t whether the drug works-it’s whether it works enough to outweigh what it takes from you.
How Do You Know If It’s Working?
Doctors don’t guess whether an antidepressant is working. They measure it. The gold standard tools are validated scales like the PHQ-9 and the Beck Depression Inventory (BDI). The PHQ-9 asks nine simple questions about sleep, energy, appetite, and hopelessness, each scored 0 to 3. A total score of 15 or higher means moderate to severe depression. After starting medication, your score should drop by at least half within six weeks. That’s the sign your treatment is on track. If it doesn’t, your doctor should adjust the dose, switch meds, or add therapy-no waiting months hoping it’ll “kick in.”Many patients never see these scales. A 2022 survey by NAMI found that 68% of people on antidepressants said their provider never used them. Instead, they were asked, “How are you feeling?”-a question too vague to track real progress. You can’t improve what you don’t measure. If your doctor skips these tools, ask for them. You can even track your own PHQ-9 scores weekly using free apps or paper forms. Just writing down your mood each week gives you clarity. One 2021 study showed patients who tracked their PHQ-9 scores reported 43% higher satisfaction with treatment.
What Side Effects Are You Actually Experiencing?
Side effects aren’t just annoying-they’re deal-breakers. Sexual dysfunction affects 61% of people on SSRIs, and many quit because no one asked. Weight gain, dry mouth, dizziness, insomnia, nausea-these aren’t “normal” side effects you just have to live with. They’re signals. The Antidepressant Side-Effect Checklist (ASEC) lists 15 common issues and rates them from 0 (none) to 4 (severe). You don’t need a doctor to use it. Keep a simple journal: write down what you feel each day. Did you feel foggy after lunch? Was your heart racing at night? Did you lose interest in things you used to love? Track it. Patterns emerge.Some side effects are serious. TCAs, for example, can mess with heart rhythms at high doses. If you’re on one and have a history of heart issues, your doctor should check your ECG before starting. If you’re on an SSRI and suddenly feel dizzy or faint, that could be low sodium-a real risk. Don’t downplay symptoms. If you’re not discussing side effects at every appointment, you’re not getting full care.
Therapeutic Drug Monitoring: The Hidden Key
Here’s something most patients don’t know: your blood can tell you if your dose is right. Therapeutic Drug Monitoring (TDM) measures exactly how much of the drug is in your bloodstream. It’s not magic-it’s science. A blood test can show if you’re getting too little (and therefore not responding) or too much (and suffering side effects). A 2022 study found that 50-70% of people who didn’t improve on antidepressants had drug levels below the therapeutic range-even when they took their pills exactly as prescribed.Why isn’t this done more often? Cost and access. A TDM test costs $50-$150 and needs a lab with specialized equipment. Only 8-12% of prescriptions include it, even though guidelines say it should be used for people who don’t respond. But if you’ve tried two or three meds with no luck, ask your doctor about TDM. It’s not experimental-it’s evidence-based. And if your doctor says no, ask for a referral to a psychiatrist who uses it.
Self-Monitoring That Actually Works
You don’t need fancy tech to monitor your progress. A simple notebook works. Each day, rate your mood on a scale from 1 to 10. Note any side effects: “Headache after lunch,” “Couldn’t sleep,” “No desire to call friends.” At the end of the week, look back. Do you see patterns? Does your mood improve after a good night’s sleep? Does nausea happen only after taking the pill on an empty stomach? This isn’t just tracking-it’s learning your body’s language.Apps like Moodfit and Sanvello help. In one 2023 trial, users who tracked daily with Moodfit had 32% better adherence than those who didn’t. But don’t get fooled by flashy features. The real value is consistency. If you log your mood three times a week, you’ll spot changes faster than waiting for a monthly doctor visit. And if you share your logs with your provider, you turn vague complaints into actionable data.
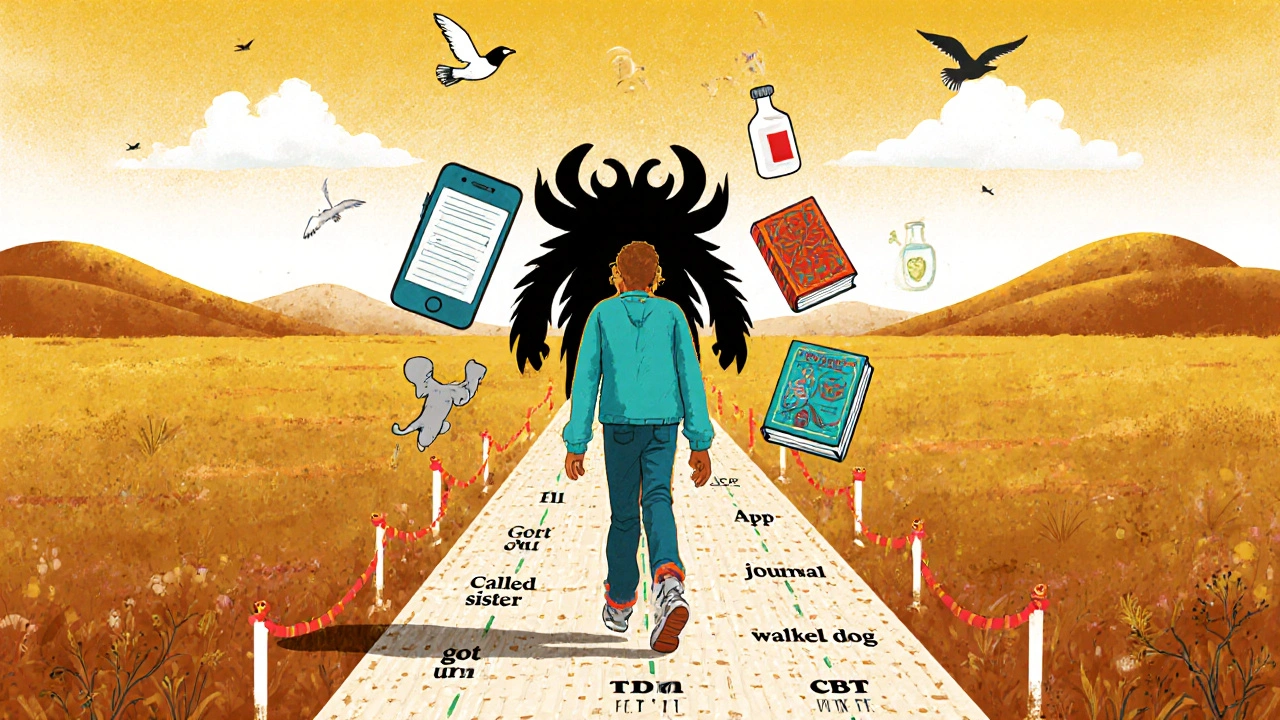
Setting Real Goals, Not Just Scores
Improvement isn’t just about lower PHQ-9 numbers. It’s about your life. A score of 8 might mean you’re not crying every day-but are you going back to work? Are you talking to your kids? Are you eating regular meals? The NIH recommends setting 3-5 specific goals when you start treatment. Examples: “Walk the dog three times a week,” “Call my sister once a week,” “Get up by 8 a.m. without hitting snooze.” These are real milestones. If your mood score drops but you’re still lying on the couch for hours, you’re not fully recovered. Track both.Some people feel better functionally before their scores improve. That’s real. One patient I know started sleeping better after two weeks-no more panic attacks at night. Her PHQ-9 was still 16, but she was finally eating again. That’s progress. Don’t let a number tell you you’re failing if your life is slowly getting better.
What to Do When It’s Not Working
If after 6-8 weeks you’re still stuck, it’s time to act. Don’t wait three months. Don’t blame yourself. The system isn’t perfect, but you can push back. Ask for:- A switch to a different class of antidepressant (e.g., from an SSRI to an SNRI or bupropion)
- Addition of therapy (CBT or interpersonal therapy have strong evidence)
- TDM to check your drug levels
- Testing for underlying issues (thyroid, vitamin D, inflammation)
- Referral to a specialist if you’re in primary care
There’s no shame in trying again. Antidepressants aren’t one-size-fits-all. What works for your friend might make you worse. That’s normal.
The Future Is Here-But You Need to Use It
New tools are arriving fast. In January 2024, the FDA cleared Rejoyn, the first digital therapeutic with built-in PHQ-9 tracking. It’s not a replacement for medication-it’s a companion. In 2023, a study showed AI could predict non-response to antidepressants as early as week two by analyzing clinical notes. And pharmacogenetic tests like GeneSight now show which drugs your body is likely to respond to-and which might cause side effects. One study found GeneSight-guided treatment reduced side effects by 30% and improved response by 20% in eight weeks.But none of this matters if you’re not involved. The system works best when you’re an active partner. You’re not just a patient. You’re the expert on your own experience. Your notes, your feelings, your daily logs-they’re data points that can change your treatment.
Final Thoughts: Your Voice Matters
Antidepressants are tools, not miracles. They’re not magic bullets. They’re part of a process-one that requires your input every step of the way. If you’re not being asked about side effects, if you’re not being measured, if you’re not being heard-you’re not getting the care you deserve. Use the tools. Track your mood. Ask for scales. Demand TDM if you’re stuck. Share your journal. Push for goals beyond “feel less sad.”Recovery isn’t just about a number on a scale. It’s about getting your life back. And you have the power to make sure your treatment helps you do that.
How often should I be assessed for antidepressant effectiveness?
You should be assessed every 2-4 weeks during the first 8-12 weeks of treatment. This is when most changes happen. After that, monthly check-ins are standard unless you’re adjusting medication or experiencing new side effects. The American Psychiatric Association now requires systematic monitoring at all treatment stages, so don’t accept less frequent visits if you’re still in the active treatment phase.
Can I track my own mood without an app?
Absolutely. A paper journal works just as well. Write down your mood each day on a scale of 1-10, note any side effects, and record key events (sleep quality, social interactions, stress triggers). Review it weekly. Many patients find this more honest than digital tools because there’s no algorithm judging their entries. The goal is consistency, not tech.
Why do some people get side effects and others don’t?
It comes down to genetics, metabolism, and individual brain chemistry. Some people break down antidepressants quickly and need higher doses; others process them slowly and get side effects at standard doses. Pharmacogenetic tests like GeneSight can identify these differences, but even without them, your body gives clues. If you’ve had bad reactions to other meds in the past, tell your doctor. That’s valuable data.
Is it normal to feel worse before feeling better?
Some people do, especially in the first 1-2 weeks. Increased anxiety, nausea, or insomnia can happen as your brain adjusts. But if you feel significantly worse after 2 weeks-like having suicidal thoughts or extreme agitation-call your doctor immediately. That’s not normal adjustment; that’s a red flag. Most people don’t get worse, but if you do, it’s not a sign you’re failing-it’s a sign your treatment needs adjusting.
What if my doctor won’t use PHQ-9 or TDM?
You have the right to ask for evidence-based care. If your provider refuses, say: “I’ve read that using PHQ-9 improves outcomes by 50-60%. Can we try it?” If they still say no, consider finding a new provider. Psychiatrists and specialized mental health clinics are far more likely to use these tools than general practitioners. Your recovery depends on your active participation-you’re not just a patient, you’re a partner in your care.
How long should I stay on an antidepressant if it’s working?
Once you’ve reached remission (PHQ-9 score below 5), guidelines recommend staying on the medication for at least 6-12 months to prevent relapse. For people with recurrent depression, longer-term use-sometimes years-is common and safe. Stopping too soon is one of the biggest reasons depression returns. Never stop abruptly. Always taper under medical supervision.
Can I combine antidepressants with therapy?
Yes-and it’s often the most effective approach. Studies show that combining antidepressants with cognitive behavioral therapy (CBT) leads to higher remission rates than either alone. Therapy helps you change thought patterns and behaviors that keep depression going. Even if you’re on medication, therapy gives you tools to stay well long-term. Don’t see them as competing-they’re teammates.


Written by Connor Back
View all posts by: Connor Back