PSA Level & BPH Impact Calculator
Enter your age and prostate volume, then click "Estimate PSA Level"
How It Works
This calculator estimates potential PSA elevation due to BPH using:
- Age-specific normal ranges
- Estimated PSA increase from prostate volume (0.1 ng/mL per 10 cc)
- BPH-related increase of 0.5-2 ng/mL
Most men over 50 hear the phrase "PSA test" and wonder if it matters for an enlarged prostate. The truth is that PSA testing can help doctors tell whether a benign growth is causing trouble, but it also brings a handful of interpretive challenges. Below you’ll find a step‑by‑step guide to what the test measures, how BPH affects PSA numbers, and what you should do with the results.
Quick Take
- PSA measures a protein from the prostate; higher levels don’t automatically mean cancer.
- Benign Prostatic Hyperplasia (BPH) often raises PSA by 0.5-2ng/mL.
- Age‑specific PSA ranges improve accuracy for men 50-80.
- Combine PSA with digital rectal exam (DRE) and symptom scores for better decision making.
- Watch PSA velocity and density if you have BPH; sudden jumps may signal further evaluation.
Understanding PSA Testing
When doctors talk about Prostate‑Specific Antigen (PSA) testing is a blood test that measures the amount of PSA protein released by the prostate gland, they’re looking for a simple number that can flag abnormalities. The test draws a few milliliters of blood, runs it through an immunoassay, and reports the concentration in nanograms per milliliter (ng/mL). The assay is highly reproducible, but the interpretation depends on age, prostate volume, and any inflammation.
What PSA Levels Mean
Traditional cut‑offs (≤4ng/mL as “normal”) are outdated because a healthy 45‑year‑old may have a PSA of 1.5ng/mL, while a 75‑year‑old with a 30cc prostate might sit at 3.5ng/mL without disease. Modern guidelines use age‑specific ranges:
- 45-49yr: ≤2.5ng/mL
- 50-59yr: ≤3.5ng/mL
- 60-69yr: ≤4.5ng/mL
- 70-79yr: ≤6.5ng/mL
These ranges account for the gradual increase in prostate volume that comes with age.
Benign Prostatic Hyperplasia (BPH) Basics
Benign Prostatic Hyperplasia is a non‑cancerous enlargement of the prostate gland that compresses the urethra and disrupts urine flow. Most men develop some degree of BPH after 40, and about 30% experience moderate to severe urinary symptoms by age 70. Symptoms are captured by the International Prostate Symptom Score (IPSS), a questionnaire that grades frequency, urgency, weak stream, and nocturia.
Diagnosis usually involves a physical exam, urine studies, and imaging (transrectal ultrasound) to estimate prostate size. PSA isn’t required for diagnosis, but it becomes relevant when clinicians need to differentiate BPH‑related PSA elevation from possible cancer.
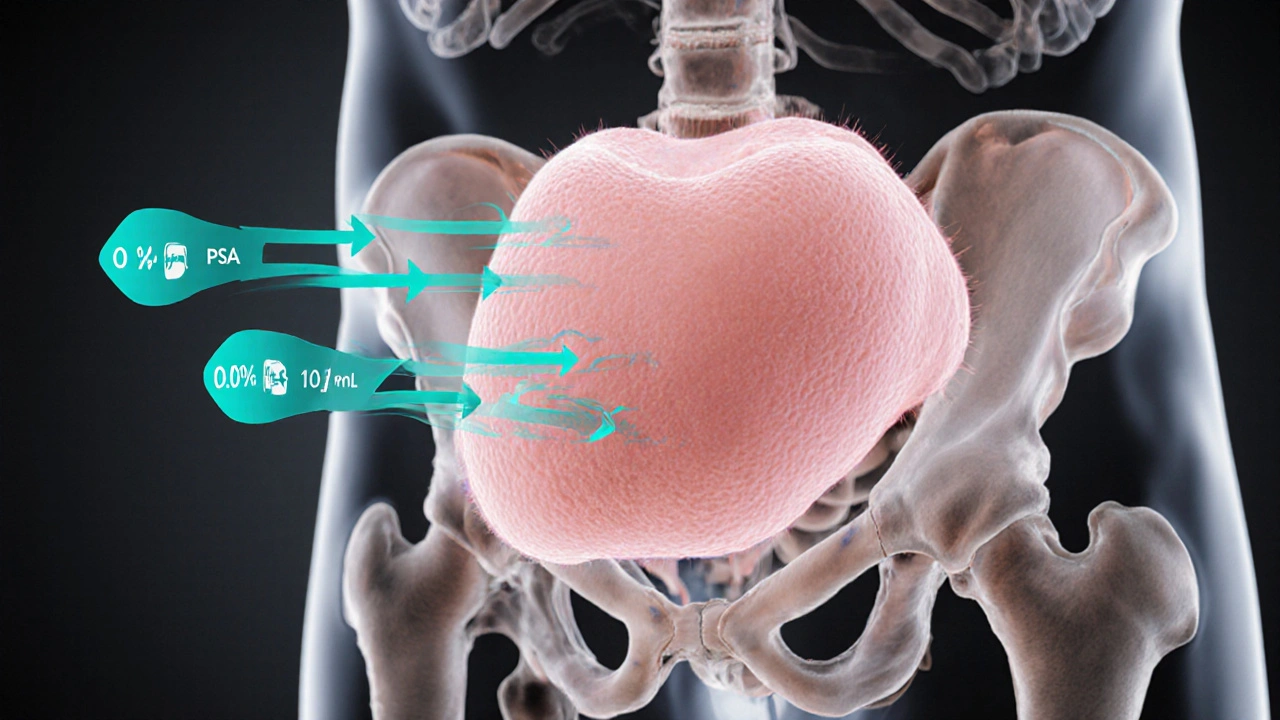
How PSA Testing Interacts With BPH
Enlarged prostate tissue produces more PSA, so BPH often lifts the baseline number by 0.5-2ng/mL. Researchers have shown that each additional 10cc of prostate volume can increase PSA by roughly 0.1ng/mL. This relationship leads to three practical uses of PSA in BPH:
- Baseline Screening: Establishing an initial PSA helps track future changes.
- Monitoring Growth: A steady rise (PSA velocity >0.75ng/mL per year) may indicate rapid gland growth.
- Rule‑out Cancer: When PSA stays modest (<4ng/mL) and DRE is normal, the likelihood of cancer is low, allowing focus on BPH therapy.
However, relying on PSA alone can miss aggressive cancers that hide behind a “normal” BPH‑related PSA. That’s why clinicians combine PSA with other tools.
Comparing PSA With Other Evaluation Tools
| Test | What It Measures | Strengths for BPH | Limitations |
|---|---|---|---|
| PSA testing | Serum PSA concentration | Quantitative, tracks trends over time | Elevated by both BPH and cancer |
| Digital Rectal Exam (DRE) | Palpation of prostate texture | Detects nodules, easy bedside tool | Subjective, limited sensitivity for early cancer |
| PSA density | PSA divided by prostate volume (ng/mL/cc) | Adjusts PSA for gland size, better cancer discrimination | Requires accurate volume measurement (ultrasound) |
| PSA velocity | Rate of PSA change per year | Highlights rapid gland expansion or occult cancer | Need multiple tests over years |
Clinical Decision‑Making With PSA in BPH
Guidelines from the American Urological Association (AUA) publish evidence‑based recommendations for prostate health suggest the following algorithm for men with symptomatic BPH:
- Obtain baseline PSA and IPSS.
- If PSA < 4ng/mL and DRE normal, proceed with BPH medical therapy (alpha‑blockers, 5‑alpha‑reductase inhibitors).
- If PSA > 4ng/mL or DRE abnormal, calculate PSA density; a density >0.15ng/mL/cc warrants referral for prostate MRI.
- Track PSA annually; a velocity >0.75ng/mL/year or a jump of >2ng/mL in six months triggers repeat imaging and possible biopsy.
This flow balances avoiding unnecessary biopsies while catching aggressive disease early.
Potential Harms and How to Mitigate Them
Over‑testing can cause anxiety, lead to invasive biopsies, and increase healthcare costs. To keep PSA useful:
- Explain to patients that PSA is a screening marker, not a definitive diagnosis.
- Use age‑adjusted reference ranges to reduce false‑positives.
- Consider a “PSA reflex” protocol where only men with values above age‑specific thresholds get further work‑up.
By applying these safeguards, clinicians maintain PSA’s value without overburdening the patient.
Practical Checklist for Patients and Providers
- Record baseline PSA, prostate volume (if known), and IPSS score.
- Schedule DRE at the same visit as PSA if not done recently.
- Review medications that can falsely elevate PSA (e.g., 5‑alpha‑reductase inhibitors) and pause them 6 weeks before testing when safe.
- Set a follow‑up interval: 12 months for stable PSA < 4ng/mL; 6 months if PSA is trending upward.
- Discuss lifestyle factors-diet, exercise, and weight loss-that may modestly lower PSA levels.
Frequently Asked Questions
Can PSA be normal if I have BPH?
Yes. Many men with moderate BPH have PSA values within age‑specific limits. In those cases, PSA is mainly used to monitor trends rather than to confirm BPH.
What PSA level should prompt a prostate biopsy?
A single cutoff isn’t enough. Typically, PSA >4ng/mL combined with an abnormal DRE, PSA density >0.15ng/mL/cc, or velocity >0.75ng/mL/year leads clinicians to recommend MRI and possibly a targeted biopsy.
Does medication for BPH affect PSA results?
5‑alpha‑reductase inhibitors can cut PSA by about 50% after six months. If you’re on such medication, doctors usually double the measured PSA to estimate the untreated level.
How often should I get my PSA checked if I have BPH?
Annual testing is common for stable PSA under 4ng/mL. If PSA is borderline or rising, a six‑month interval helps catch significant changes early.
Is a high PSA always a sign of prostate cancer?
No. Inflammation, infection, recent ejaculation, or BPH can all raise PSA. That’s why a comprehensive evaluation-including DRE, imaging, and sometimes repeat PSA-provides a clearer picture.


Written by Connor Back
View all posts by: Connor Back