Chronic Diarrhea & Ulcerative Colitis Risk Checker
This tool helps assess whether your symptoms might be related to ulcerative colitis. Answer the questions below to get personalized insights.
Chronic diarrhea and ulcerative colitis often appear as separate problems, but they share a hidden link that many patients overlook.
- Both conditions involve inflammation of the colon.
- Immune system dysfunction and gut‑microbiome changes are common triggers.
- Symptoms can overlap, making diagnosis tricky.
- Early testing (colonoscopy, stool studies) can spot the connection.
- Targeted diet and medication help control both issues.
What Is Chronic Diarrhea?
When the bowels move more than three times a day for four weeks or longer, doctors call it chronic diarrhea a persistent condition marked by frequent, watery stools that lasts for at least a month. It isn’t just a nuisance; prolonged fluid loss can lead to dehydration, electrolyte imbalance, and weight loss.
Common causes include infections, food intolerances, medications, and diseases that affect the large intestine. Among the more serious culprits are inflammatory bowel diseases (IBD) such as ulcerative colitis and Crohn’s disease.
Understanding Ulcerative Colitis
Ulcerative colitis a chronic inflammatory bowel disease that exclusively affects the lining of the colon and rectum often presents with abdominal pain, bloody stools, and urgency. The inflammation starts in the rectum and can spread upward, eroding the mucosal layer and forming ulcers.
Unlike Crohn’s disease, ulcerative colitis does not penetrate deeper layers of the bowel wall, which means the risk of strictures is lower, but the chance of flare‑ups remains high.
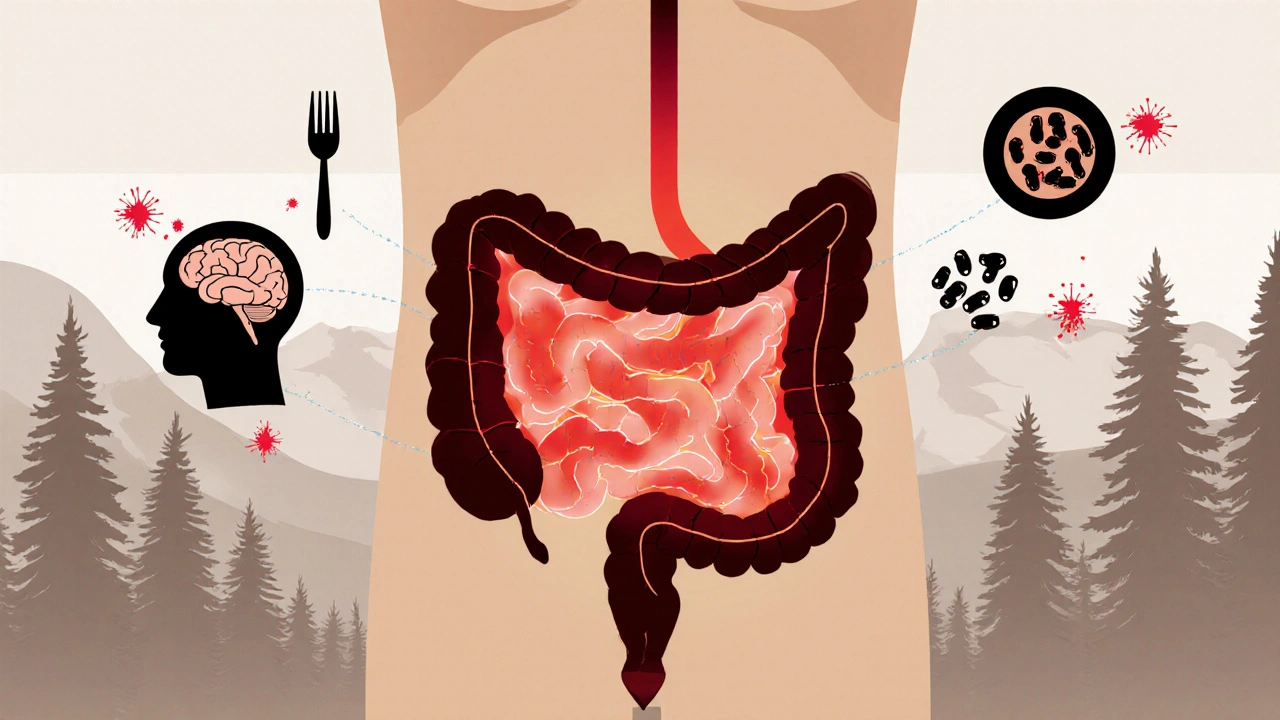
Shared Biological Pathways
Both chronic diarrhea and ulcerative colitis tap into three main biological systems:
- Immune system the body’s defense network that can mistakenly attack gut tissue in IBD. In ulcerative colitis, immune cells release cytokines that inflame the colon, increasing fluid secretion and causing diarrhea.
- Gut microbiome the community of trillions of bacteria living in the intestines. Dysbiosis-an imbalance of good and bad bacteria-has been linked to both diarrhea and ulcerative colitis, amplifying inflammation.
- Colon the final segment of the digestive tract where water is reabsorbed. When the colon’s lining is damaged, it can’t reclaim water efficiently, leading to watery stools.
These overlapping mechanisms explain why many ulcerative colitis patients complain of chronic diarrhea, even when the disease is technically “in remission.”
Diagnosing the Overlap
Because the symptoms look alike, doctors use a combination of tests to pinpoint the cause.
| Test | What It Shows | Relevance |
|---|---|---|
| Colonoscopy | Visualizes inflammation, ulcers, and bleeding | Gold standard for ulcerative colitis; can rule out other causes of diarrhea |
| Stool Culture & PCR | Detects bacterial, viral, or parasitic infections | Helps eliminate infectious causes of chronic diarrhea |
| Fecal Calprotectin | Measures inflammatory protein in stool | Elevated levels suggest IBD rather than functional diarrhea |
| Blood Tests (CBC, CRP) | Shows anemia, inflammation, and immune activity | Supports a systemic view of disease activity |
When labs reveal high calprotectin along with persistent watery stools, physicians often suspect an underlying ulcerative colitis flare, even if visible blood is absent.
Treatment Strategies That Hit Both Targets
Managing chronic diarrhea caused by ulcerative colitis involves three angles: controlling inflammation, restoring gut balance, and adjusting diet.
- Anti‑inflammatory meds: 5‑ASA compounds (mesalamine), steroids, or biologics (infliximab) reduce immune‑driven inflammation, which in turn decreases stool frequency.
- Probiotics & Prebiotics: Specific strains like Bifidobacterium and Lactobacillus rhamnosus have shown promise in reducing diarrhea episodes by reshaping the microbiome.
- Low‑FODMOs diet: Cutting fermentable carbs can lessen gas‑producing bacteria, easing both abdominal pain and loose stools.
- Hydration & electrolytes: Oral rehydration solutions (ORS) replace lost sodium and potassium, preventing dehydration during flare‑ups.
Patients who combine medication with dietary tweaks report up to a 40% reduction in daily bowel movements compared with medication alone.
When to Seek Medical Attention
Not every bout of diarrhea warrants a colonoscopy, but some red flags signal an urgent need for professional evaluation:
- Stools contain blood or mucus.
- Weight loss exceeds 5% of body weight in a month.
- Fever above 101°F (38.5°C) accompanies diarrhea.
- Persistent dehydration despite oral fluids.
- New onset of severe abdominal pain.
If you notice any of these signs, schedule a gastroenterology appointment promptly. Early detection of ulcerative colitis can prevent complications like strictures or colorectal cancer.
Living with the Dual Challenge
Understanding that chronic diarrhea can be a symptom of ulcerative colitis changes the entire management plan. Instead of treating the diarrhea as an isolated issue, patients and doctors work together to keep inflammation in check.
Practical habits that help:
- Track stool frequency, consistency, and triggers in a journal.
- Maintain a regular medication schedule; never skip a dose during a “quiet” period.
- Stay hydrated with electrolyte‑balanced drinks, especially during hot Tampa summers.
- Engage in low‑impact exercise (walking, swimming) to support gut motility without over‑stimulating the colon.
- Join a support group-sharing experiences often surfaces coping tricks that doctors haven’t mentioned.
With the right combination of medical care and lifestyle tweaks, most people achieve a stable remission where diarrhea becomes an occasional, manageable symptom rather than a daily battle.

Frequently Asked Questions
Can chronic diarrhea be the first sign of ulcerative colitis?
Yes. Many patients notice persistent watery stools weeks before any visible blood appears. If diarrhea lasts more than four weeks, a screening colonoscopy is advisable.
Is it safe to use over‑the‑counter anti‑diarrheal meds if I have ulcerative colitis?
Generally not. Drugs like loperamide can mask symptoms and potentially worsen inflammation. Always check with your gastroenterologist before self‑medicating.
How does the gut microbiome influence both conditions?
An unhealthy microbiome produces excess gas and toxins that irritate the colon lining, triggering both diarrheal episodes and inflammatory pathways seen in ulcerative colitis.
What dietary changes reduce diarrhea during a flare?
A low‑FODMOs plan, avoiding caffeine, alcohol, and high‑fat foods, while increasing bland proteins (chicken, fish) and soluble fiber (oats) often helps control stool frequency.
Can stress worsen chronic diarrhea and ulcerative colitis?
Stress activates the hypothalamic‑pituitary‑adrenal axis, which can increase gut permeability and inflammatory cytokine release, making both conditions flare up.
Are there any non‑invasive tests that can differentiate between the two?
Fecal calprotectin is a reliable marker-high levels point toward an inflammatory cause like ulcerative colitis, while normal levels suggest a functional or infectious diarrhea.


Written by Guy Boertje
View all posts by: Guy Boertje