Asthma Action Plan Builder
Your Personalized Asthma Action Plan
For
Personal Best Peak Flow: L/min
Medication:
Known Triggers:
Symptoms occur ≤ twice a week, no night awakenings.
Continue daily controller medication.
Symptoms > twice a week, or a single night awakening.
Use - 2 puffs every 4-6 hours.
Severe breathlessness, speaking in short phrases, or peak flow < 50% of personal best.
Take 4 puffs of , call emergency services, and sit upright.
- Review this plan with your healthcare provider at least twice a year.
- Always carry a spare inhaler in multiple locations.
- Keep a copy of this plan at home, work, and in your bag.
Understanding asthma attacks can save lives, but many people still underestimate how quickly symptoms can turn deadly. The good news? A solid education program and community awareness can cut the risk dramatically. Below we break down what an asthma attack really is, why knowledge matters, and how you can turn that knowledge into everyday safety.
What Exactly Is an Asthma Attack?
Asthma is a chronic respiratory condition that makes the airways overly sensitive to certain stimuli. When a trigger hits, the airway muscles tighten, the lining swells, and mucus builds up, leading to an asthma attack, a sudden worsening of symptoms that can include wheezing, shortness of breath, chest tightness, and coughing. Most attacks develop within minutes, and if untreated, can progress to respiratory failure.
Key physiological facts (based on CDC data from 2024):
- Nearly 25million people in the U.S. have asthma.
- About 1.5million emergency department visits each year are due to asthma attacks.
- Children under 5 experience the highest rate of hospitalization.
Why Education Beats Panic
When a person knows the early warning signs-like a sudden cough at night or a feeling of tightness in the chest-they’re far more likely to act before the attack spirals. Studies from the National Asthma Education and Prevention Program (NAEPP) show that patients who complete an asthma education course reduce emergency visits by up to 30%.
Education works on three levels:
- Recognition: Learning to spot subtle symptoms.
- Response: Knowing the exact steps to take, such as using a rescue inhaler correctly.
- Prevention: Identifying and avoiding personal triggers.
Without this knowledge, even a well‑managed medication routine can fail during a rapid attack, leaving the person scrambling for help.
Core Components of Effective Asthma Education
Most reputable programs cover the same five pillars. Below is a quick checklist you can use to evaluate any class, website, or pamphlet.
- Understanding triggers: From pollen to pet dander, the guide should list common culprits.
- Proper inhaler technique: Incorrect use reduces drug delivery by up to 50%.
- Peak flow monitoring: Using a peak flow meter helps track airway narrowing days before symptoms appear.
- Asthma action plan: A personalized, written plan that outlines step‑by‑step actions for mild, moderate, and severe symptoms.
- Environmental control: Practical steps to reduce indoor allergens, such as using HEPA filters and regular mattress encasings.
When these elements are bundled together, patients report greater confidence and lower anxiety during flare‑ups.
Building Your Personal Asthma Action Plan
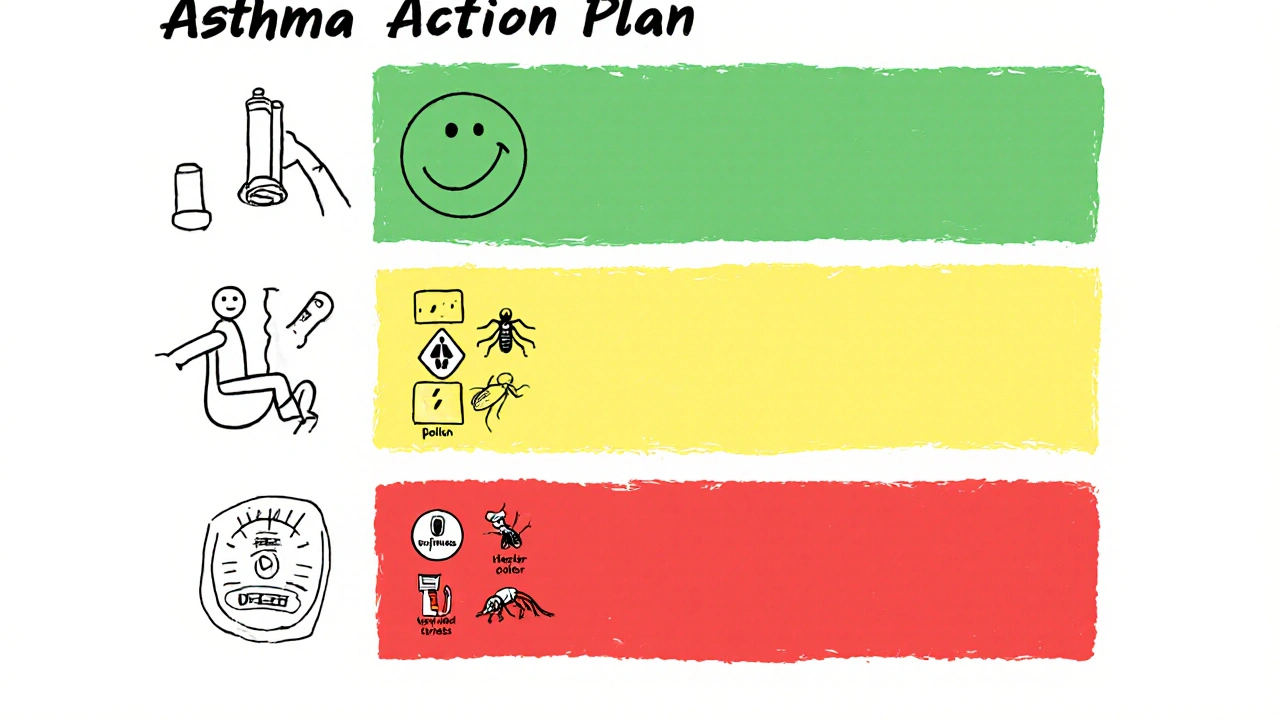
A well‑crafted plan is the single most powerful tool you’ll have on hand. It should be a single page, color‑coded, and easily readable. Below is a template you can copy:
- Green zone (good control): Symptoms ≤ twice a week, no night awakenings. Continue daily controller medication.
- Yellow zone (caution): Symptoms > twice a week, or a single night awakening. Use a rescue inhaler (e.g., albuterol) - 2 puffs every 4‑6hours.
- Red zone (danger): Severe breathlessness, speaking in short phrases, or peak flow < 50% of personal best. Take 4 puffs of rescue inhaler, call emergency services, and sit upright.
Keep a copy at home, work, and in your bag. Review it with your healthcare provider at least twice a year.
Common Triggers and How to Tame Them
Not all triggers are obvious. Some people react to cold air, strong odors, or even emotional stress. The table below breaks down the most frequent culprits and practical mitigation steps.
| Trigger | Typical Sources | Mitigation |
|---|---|---|
| Allergens | Pollen, dust mites, pet dander | Use HEPA filters, wash bedding weekly, keep pets out of bedrooms |
| Air Pollution | Vehicle exhaust, industrial smoke | Check AQI, stay indoors on high‑pollution days, wear N95 mask if needed |
| Cold Air | Winter outdoor activities | Wear a scarf over mouth, warm up indoors before exercise |
| Exercise | Running, aerobics | Warm‑up gradually, use inhaler 15minutes before activity |
| Strong Odors | Perfumes, cleaning agents | Choose fragrance‑free products, ventilate rooms well |
| Stress | Work pressure, anxiety | Practice breathing exercises, yoga, or mindfulness |
Tracking which triggers set you off (through a symptom diary or a smartphone app) sharpens your action plan over time.
The Role of Community Awareness
Education isn’t just an individual task. When schools, workplaces, and local governments spread accurate information, the collective risk drops. Here’s why community outreach matters:
- Early detection: Teachers trained to notice wheezing can request medical assistance before a child’s condition worsens.
- Reduced stigma: When friends understand that an inhaler is a life‑saving device-not a sign of weakness-they’re more likely to support usage in public.
- Policy change: Cities that ban smoking in public parks see a 12% decline in asthma-related ER visits.
Many towns now host “Asthma Awareness Week,” offering free peak flow checks, inhaler workshops, and educational booths at community centers. If your area lacks such events, consider partnering with local clinics or pharmacy chains to start one.
Practical Steps to Raise Awareness Today
You don’t need a megaphone to make a difference. Below are five actions you can take right now:
- Share a one‑page fact sheet: Print a concise handout on triggers and keep it in your office lobby.
- Host a mini‑workshop: Invite a respiratory therapist to demonstrate inhaler technique for families.
- Leverage social media: Post a short video of how to use a peak flow meter; tag local health departments.
- Advocate for school policies: Ask the PTA to include an asthma emergency kit in every classroom.
- Volunteer for local health fairs: Offer free symptom screenings and distribute action plan templates.
Even a single shared tip can spark a chain reaction that protects dozens of people.
When to Seek Professional Help
Even the best‑educated asthma patient should know when self‑management isn’t enough. Contact a healthcare professional if you notice any of these red flags:
- Need to use rescue inhaler more than twice a week.
- Nighttime awakenings due to breathing difficulty more than twice a month.
- Peak flow reading consistently below 80% of personal best.
- New or worsening symptoms after a change in medication.
Regular follow‑ups (at least twice a year) allow your doctor to adjust controller doses and ensure your action plan stays current.
Key Takeaways
Education and awareness turn a potentially fatal asthma attack into a manageable event. By recognizing early symptoms, mastering inhaler use, monitoring peak flow, and keeping a personalized action plan, you cut emergency visits dramatically. Extending that knowledge to families, schools, and workplaces builds a safety net that protects everyone.

Frequently Asked Questions
What is the difference between a rescue inhaler and a controller medication?
A rescue inhaler (like albuterol) works within minutes to relax airway muscles during an acute flare‑up. Controller medications (often inhaled corticosteroids) are taken daily to reduce inflammation and prevent attacks. Using a rescue inhaler too often may signal that your controller plan needs adjustment.
How often should I replace my peak flow meter?
Most manufacturers recommend replacement every 12‑18 months or sooner if the reading seems inconsistent. Keep a spare in your emergency kit.
Can stress really trigger an asthma attack?
Yes. Stress releases hormones that can cause airway tightening. Practicing deep‑breathing or mindfulness reduces the likelihood of stress‑related attacks.
What should I do if my inhaler runs out during an attack?
If you have a spare inhaler, use it immediately. If not, call emergency services while taking any remaining medication. Always keep a backup inhaler in a separate location.
Are there any new asthma treatments on the horizon?
Biologic therapies targeting specific inflammatory pathways (like dupilumab) have shown promise for severe asthma. These are prescribed by specialists after standard treatments fail.


Written by Guy Boertje
View all posts by: Guy Boertje