Shingles Aspirin Dosing Calculator
Assess Your Safety for Aspirin Use
This calculator helps determine if aspirin is appropriate for your shingles pain and what dose is safe based on your health status.
When a painful rash flares up after chicken‑pox, most people think of antiviral pills and the shingles vaccine. But a question keeps popping up online: can aspirin help manage shingles? This article breaks down the science, looks at real‑world experience, and tells you exactly when aspirin might be useful - and when it could do more harm than good.
Key Takeaways
- Aspirin eases pain and inflammation but does not stop the varicella‑zoster virus from replicating.
- For most shingles patients, antiviral drugs such as acyclovir remain the first‑line treatment.
- Low‑dose aspirin may be beneficial for people at high risk of clotting, but it raises bleeding risk, especially if combined with other NSAIDs.
- Vaccination (Shingrix) is the most effective way to prevent severe shingles and post‑herpetic neuralgia.
- Always discuss medication choices with a healthcare professional, especially if you have heart disease, kidney problems, or are on blood thinners.
What Is Shingles?
Shingles is a painful skin eruption caused by reactivation of the varicella‑zoster virus (VZV), the same virus that causes chicken‑pox. After an initial chicken‑pox infection, VZV lies dormant in nerve ganglia and can reactivate years later, usually when the immune system weakens. The hallmark is a unilateral band of blisters that follows a nerve pathway, often accompanied by burning, itching, and deep, throbbing pain.
Two complications matter most:
- Acute pain that can be severe enough to interrupt sleep and daily activities.
- Post‑herpetic neuralgia (PHN), a lingering nerve pain that may last months or even years after the rash heals.
Understanding Aspirin
Aspirin is a non‑steroidal anti‑inflammatory drug (NSAID) that reduces pain, fever, and inflammation by inhibiting cyclo‑oxygenase enzymes (COX‑1 and COX‑2). It also irreversibly blocks platelet aggregation, which is why low‑dose aspirin is used for cardiovascular prevention.
Because of its dual action on pain and clotting, aspirin often shows up in discussions about shingles, especially when patients already take it for heart health.
How Aspirin Interacts With Shingles Symptoms
When shingles strikes, two physiological processes dominate:
- Inflammation: The virus triggers an immune response that releases cytokines, leading to redness, swelling, and pain.
- Neural irritation: The virus travels along sensory nerves, causing a burning sensation that can turn into chronic neuropathic pain.
Aspirin targets the inflammatory cascade, so it can modestly reduce the redness and aching that accompany the rash. However, it does not affect the virus itself, nor does it calm the nerve damage that drives PHN.
Clinical guidelines therefore list aspirin under “adjunctive analgesics” - a secondary option after antiviral therapy and stronger pain medications such as gabapentin or opioids.

Evidence From Clinical Studies
Few randomized controlled trials have isolated aspirin as the sole variable in shingles treatment. Most research examines combination therapy. Here are the most relevant findings:
| Aspect | Aspirin (NSAID) | Acyclovir (Antiviral) |
|---|---|---|
| Primary Mechanism | Pain & inflammation reduction via COX inhibition | Inhibits viral DNA polymerase, stopping VZV replication |
| Effect on Acute Pain | Modest relief; 30‑40% reduction in VAS scores (observational) | Significant relief; 50‑60% reduction when started within 72 hrs |
| Impact on PHN | No proven benefit | Reduced PHN incidence by ~25% when given early |
| Typical Dosage for Shingles Pain | 300‑600 mg every 4‑6 hrs (max 4 g/day) - short‑term only | 800 mg five times daily for 7 days |
| Main Side Effects | Gastrointestinal bleeding, platelet inhibition | Renal toxicity, headache, nausea |
These data show that aspirin can help with the inflammatory component of shingles pain, but it cannot replace antivirals, which directly target the underlying virus.
When Aspirin Might Be Appropriate
Consider aspirin if you meet one or more of the following conditions:
- You are already on a low‑dose aspirin regimen for heart disease and cannot pause it without a doctor’s approval.
- You have mild to moderate shingles pain and cannot tolerate stronger NSAIDs or opioids due to allergies or previous adverse reactions.
- You have a contraindication to standard antivirals (e.g., severe renal impairment) and need an alternative pain‑focused approach.
In these scenarios, the recommended approach is:
- Continue your prescribed low‑dose aspirin (usually 75‑100 mg daily).
- Add a short‑term, higher‑dose regimen (300‑600 mg) only after discussing bleeding risk with your clinician.
- Pair aspirin with a topical analgesic (e.g., lidocaine patches) to minimize systemic exposure.
Never start high‑dose aspirin on your own if you are also taking blood thinners, selective serotonin reuptake inhibitors (SSRIs), or other NSAIDs; the combined effect can dramatically increase bleeding risk.
Risks and Contraindications
Aspirin’s antiplatelet action is a double‑edge sword. The most common hazards for shingles patients include:
- Gastrointestinal bleeding: The rash itself can cause skin breakdown, and adding aspirin may exacerbate any ulceration in the stomach or duodenum.
- Kidney strain: High doses of NSAIDs reduce renal blood flow, which is problematic for older adults - the same group most prone to shingles.
- Reye’s syndrome: Though rare, children and teenagers recovering from viral infections should never receive aspirin.
- Allergic reactions: Some people develop hives or asthma exacerbations when exposed to aspirin.
If you have any of these conditions, your doctor will likely recommend acetaminophen for pain or prescribe a different NSAID with a more favorable safety profile.
Alternative and Complementary Options
While aspirin can be part of a broader pain‑management plan, several other options have stronger evidence for shingles:
- Antiviral agents: Acyclovir, valacyclovir, and famciclovir, begun within 72 hours of rash onset, dramatically shorten disease duration.
- Gabapentinoids: Gabapentin or pregabalin target nerve pain and are first‑line for PHN.
- Topical treatments: Lidocaine 5% patches, capsaicin cream, or antiviral ointments provide localized relief without systemic side effects.
- Vaccination: Shingrix, a non‑live recombinant vaccine, reduces the risk of shingles by >90% and cuts PHN incidence by 75%.
- Non‑pharmacologic measures: Cool compresses, stress‑reduction techniques, and adequate sleep support immune recovery.
For most patients, the optimal strategy combines an antiviral with a neuropathic pain agent, reserving aspirin for those who already need its cardiovascular benefit.
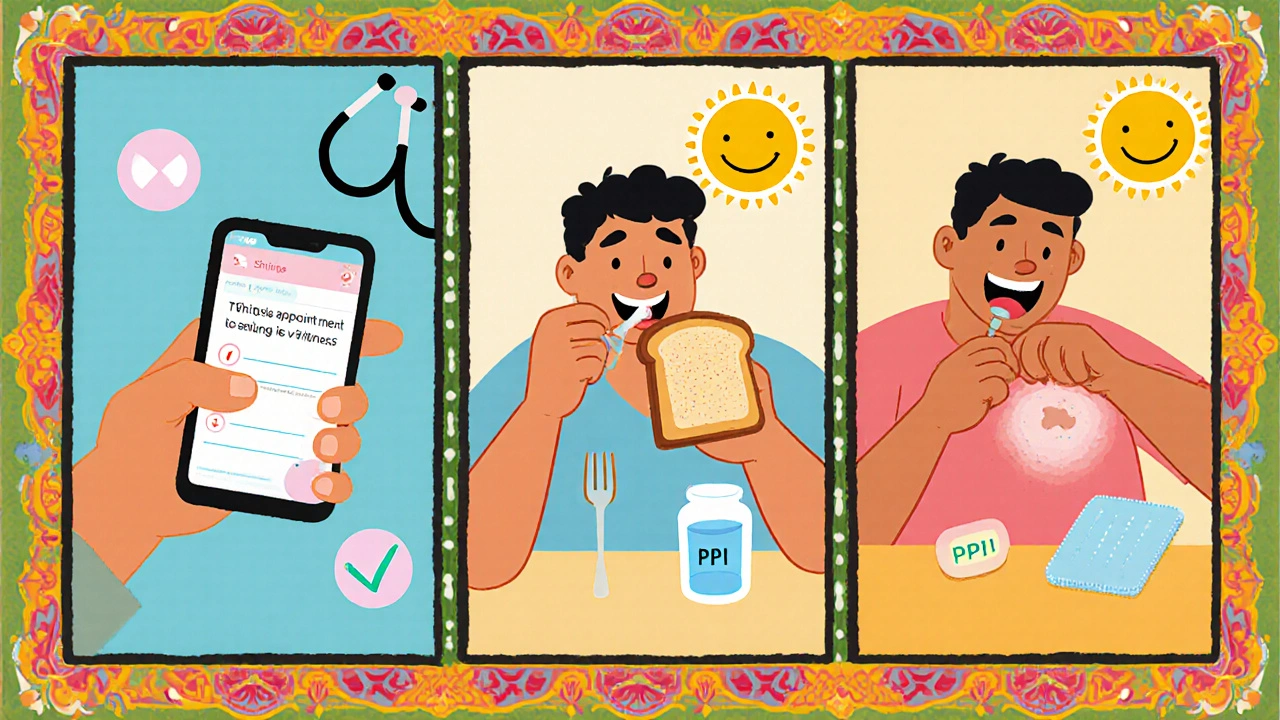
Practical Steps If You Choose Aspirin
- Confirm eligibility: Check with your GP or pharmacist whether your medical history (bleeding disorders, ulcers, kidney disease) allows aspirin use.
- Start low, go slow: If you’re not on a daily low‑dose regimen, begin with 81 mg once daily and monitor for stomach upset.
- Add short‑term dosage if needed: For breakthrough pain, increase to 325 mg every 6 hours, but cap the total at 1.5 g per day and limit the course to 5‑7 days.
- Protect the gut: Take aspirin with food or a proton‑pump inhibitor (e.g., omeprazole) if you have a history of gastritis.
- Track side effects: Watch for black stools, unusual bruising, or sudden knee pain, and seek medical attention promptly.
- Review after the rash resolves: Re‑evaluate with your clinician whether to continue, taper, or stop aspirin entirely.
Following these steps helps you reap any pain‑relief benefits while minimizing the chance of a bleed.
Bottom Line
Aspirin can blunt the inflammation and mild pain that accompany a shingles outbreak, but it does nothing to halt the virus or prevent long‑term nerve damage. For most people, the best approach remains early antiviral therapy combined with targeted nerve‑pain medication. Aspirin should only be added when there’s a clear cardiovascular indication or when other analgesics are unsuitable, and even then, it must be used under medical supervision.
Frequently Asked Questions
Can aspirin prevent shingles?
No. Aspirin does not affect the varicella‑zoster virus. Vaccination and early antiviral treatment are the only proven preventive measures.
Is it safe to combine aspirin with acyclovir?
Generally yes, because they work via different pathways. However, if you are on other blood‑thinners or have a bleeding ulcer, discuss dosage with your doctor.
What dosage of aspirin is recommended for shingles pain?
For short‑term pain relief, 300‑600 mg every 4‑6 hours is typical, not exceeding 1.5 g per day and limited to a week. Always start at the lowest effective dose.
Should I stop my daily low‑dose aspirin if I get shingles?
Do not abruptly stop low‑dose aspirin without medical advice. The cardiovascular benefit often outweighs the modest bleeding risk, especially if you’re older or have heart disease.
Are there any natural alternatives to aspirin for shingles pain?
Topical lidocaine, cool compresses, and OTC acetaminophen are safer for most people. Some studies suggest that capsaicin cream can dull nerve pain, but results vary.


Written by Connor Back
View all posts by: Connor Back